Neonatology
Session: Neonatal/Infant Resuscitation 3
294 - Implementation of PALS in a Level IV NICU
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 294
Publication Number: 294.2900
Publication Number: 294.2900
- Sc
Sandeep k. chilakala, MD
Associate Professor
University of Tennessee Health Science Center College of Medicine
Germantown, Tennessee, United States
Presenting Author(s)
Background: Neonatal Resuscitation Program (NRP) originally designed to support the transitional physiology in the delivery room has extended to Neonatal Intensive Care Unit (NICU) and beyond. NRP focuses on ventilation as the likely etiology of arrest in newborns is respiratory failure. Level IV NICUs admit infants with complex cardiac and medical conditions with extended stay up to several months. NRP may not be ideal in resuscitating such infants. Pediatric Advanced Life Support (PALS) focuses on cardiac compressions. There is lack of agreed upon criteria for implementation of PALS in the NICU. For cardiopulmonary resuscitation (CPR) events in our NICU, we implemented guidelines for using PALS
Objective: Implementing PALS during CPR in infants with PMA ≥ 48 weeks, with etiology of arrest cardiac in origin, and infants with major congenital heart defects at a level IV NICU. Compliance and effectiveness of guidelines, contributing factors, and preferred learning methods were evaluated
Design/Methods: CPR events in NICU between Aug 2022 until Aug 2023 were identified and divided in to two cohorts. PALS cohort included CPR events qualified under new guidelines and rest included in NRP cohort. Code records were reviewed retrospectively. Demographics, resuscitation methods, interventions, and outcomes were compared. A 27-questionnaire survey was sent to 38 NICU providers at 6 months and at 1 year after implementation and responses noted.
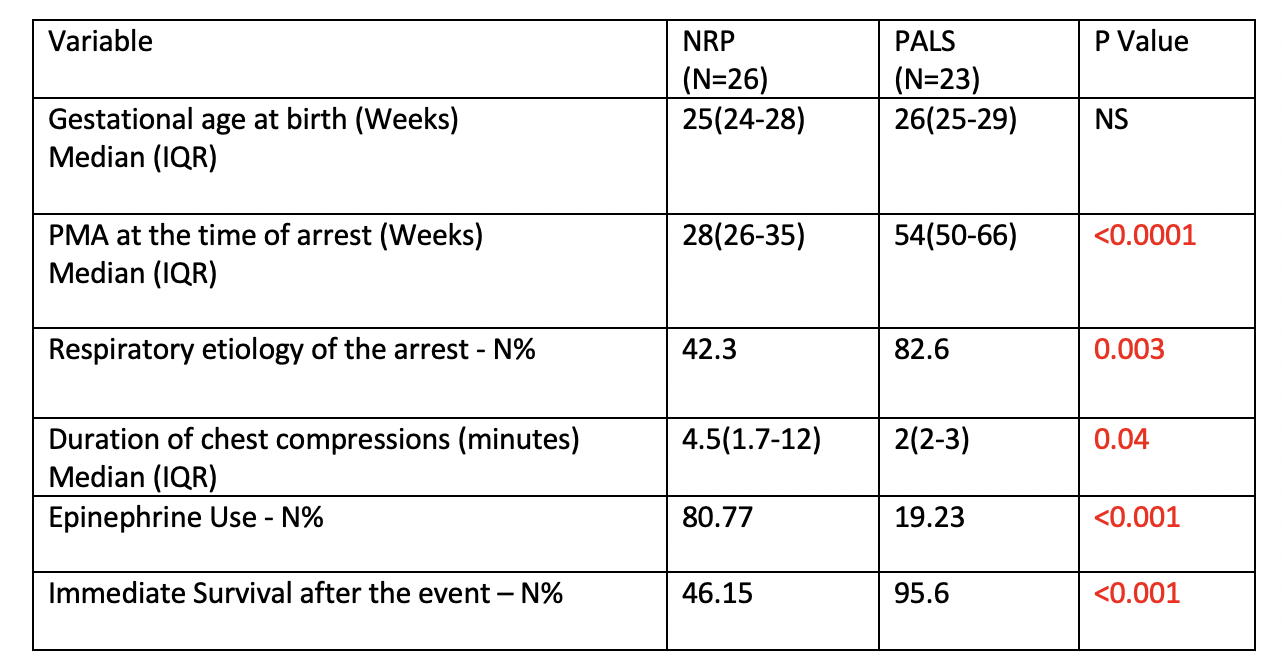
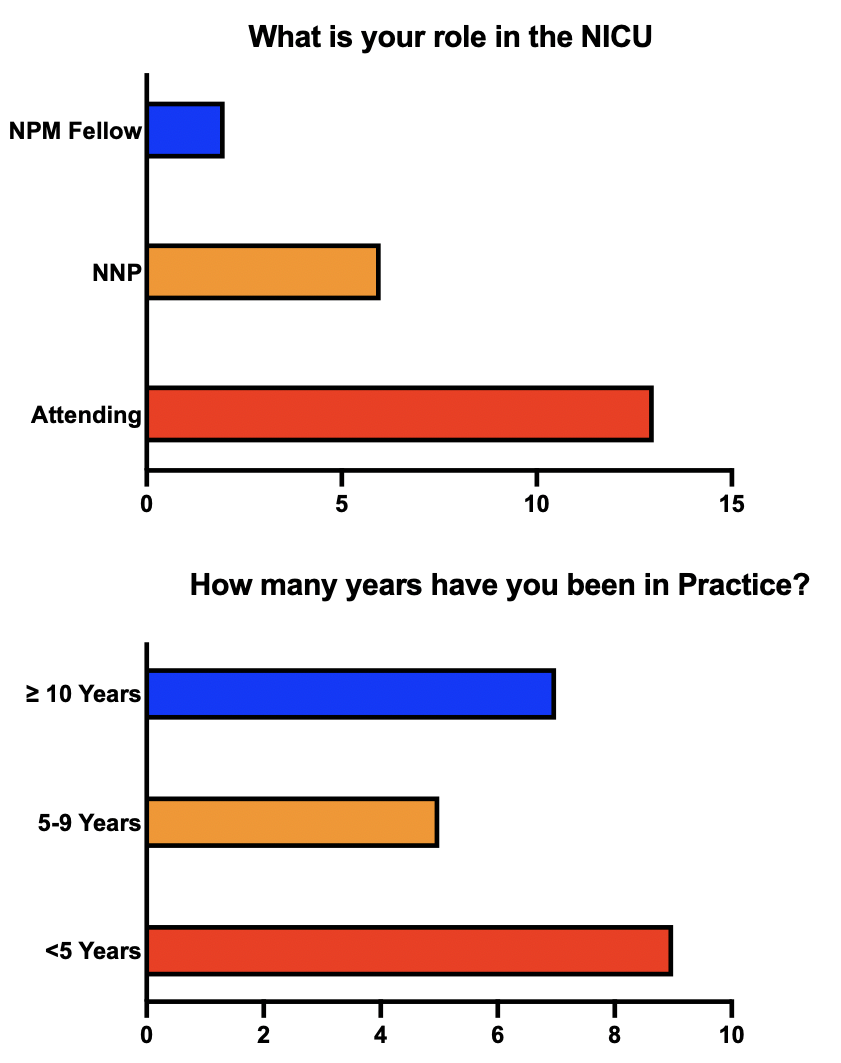
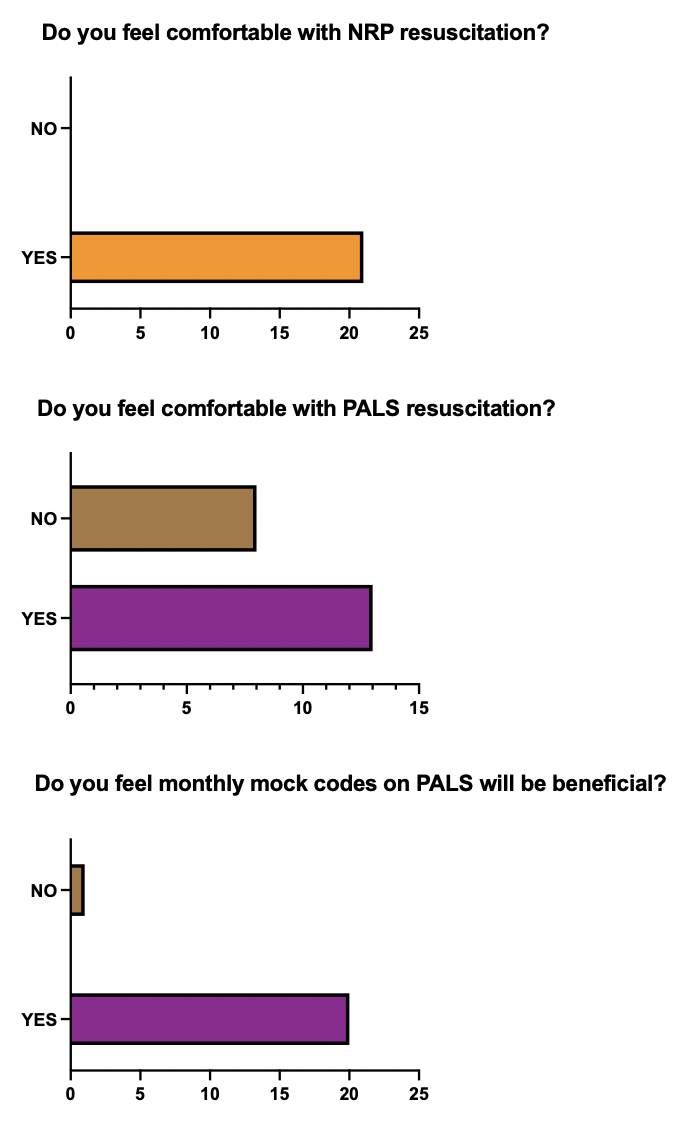
Results: 49 CPR events were identified of which, 23(47%) had PALS and 26 (53%) received NRP. Table 1 shows GA, PMA, etiology, duration, epinephrine use between the two groups. PALS group had significantly higher PMA at arrest and predominant etiology of arrest is respiratory in origin. NRP group had significantly higher use of epinephrine, longer duration of chest compressions. Immediate survival in PALS group is significantly higher. Other variables were similar. No shockable rhythms were identified.12% of the total infants admitted to the NICU qualified for PALS. Compliance to assigned algorithm is 100%. Provider survey at 1 year had 21 responses (56%) and characteristics are in Fig 1. Results indicate (Fig 2) 61 % are comfortable leading PALS code and 100% are comfortable with NRP. 95 % agree that mock codes on PALS are beneficial
Conclusion(s): We were able to successfully implement PALS in a Level IV NICU with expanding scope of care and prolonged stay. Provider comfort needs to be improved by reeducation and frequent mock codes. Simulation-based training could help in timely appropriate resuscitation and avoid variation