Neonatology
Session: Neonatal Fetal Nutrition & Metabolism 3: Enteral Nutrition
440 - Feeding Preterm Infants: An Updated Standard of Care
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 440
Publication Number: 440.2000
Publication Number: 440.2000
Enrique Gomez, MD, MSc
Assistant Professor of Pediatrics
University of Kentucky College of Medicine
Jonesboro, Arkansas, United States
Presenting Author(s)
Background: Enteral feeding practices in premature infants have changed in the last decade. However, despite significant evidence supporting earlier enteral feeds, faster advancement, and fortification, there is still not a strong recommendation to implement these findings.
Objective: To evaluate the outcomes of preterm infants after temporal changes in enteral feeding patterns at a Neonatal Intensive Care Unit (NICU).
Design/Methods: A quasi-experimental retrospective study was conducted in a level IIIA NICU in Arkansas from 2016 to 2023. Extensive feeding data and outcomes were collected by utilizing a NutritionIQ software application, NICUtrition®. Infants born between 26- and 34-weeks gestational age (GA) were included. Infants with congenital defects, deceased and with incomplete data were excluded.
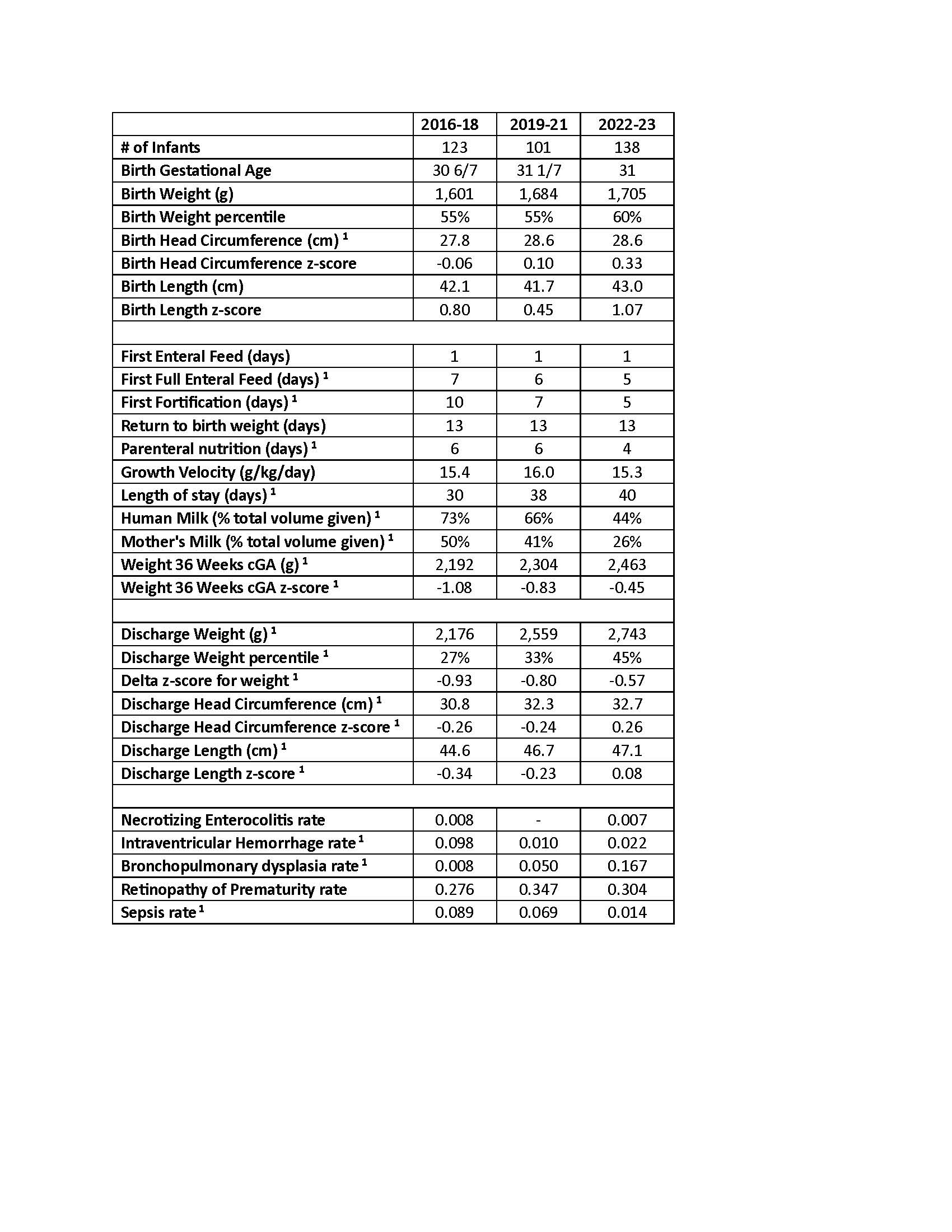
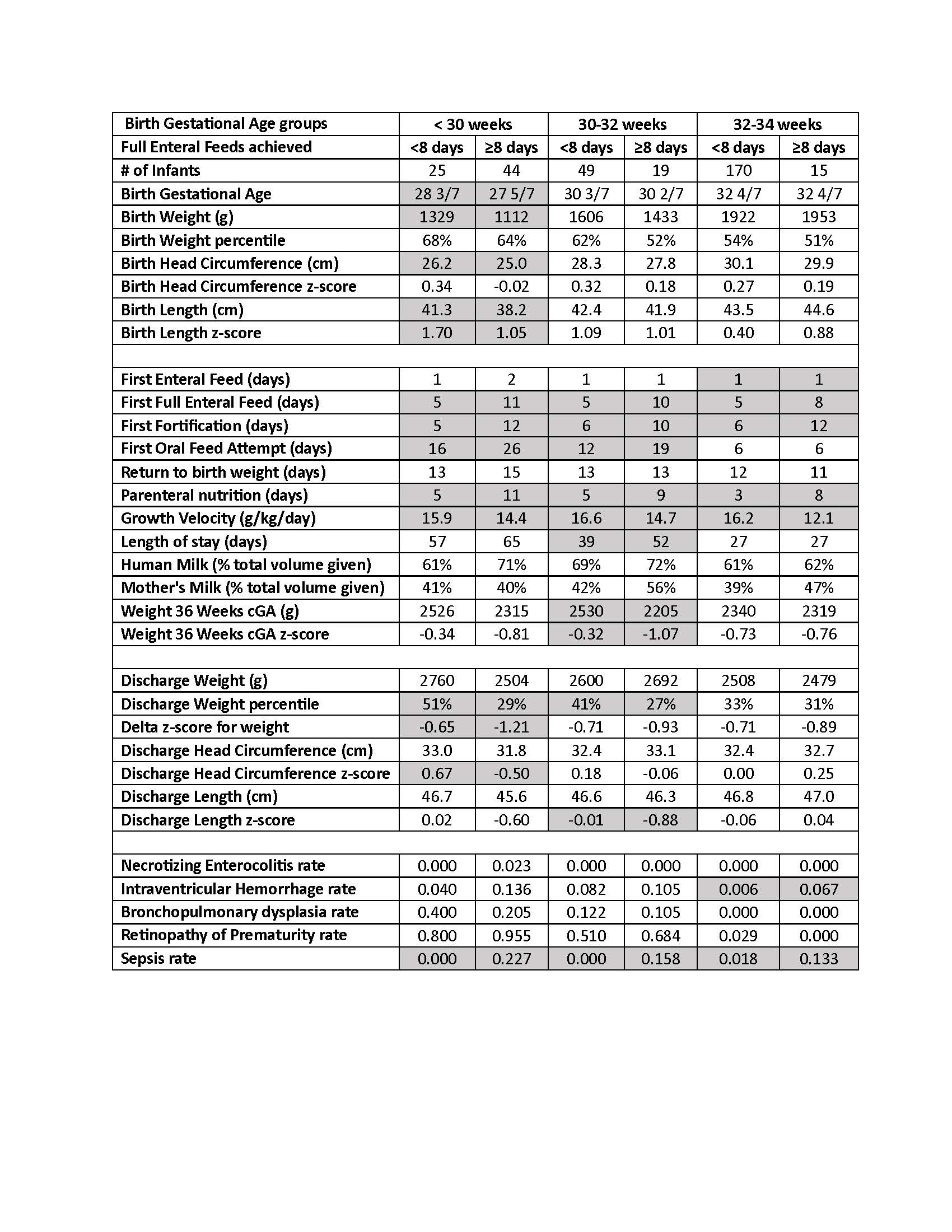
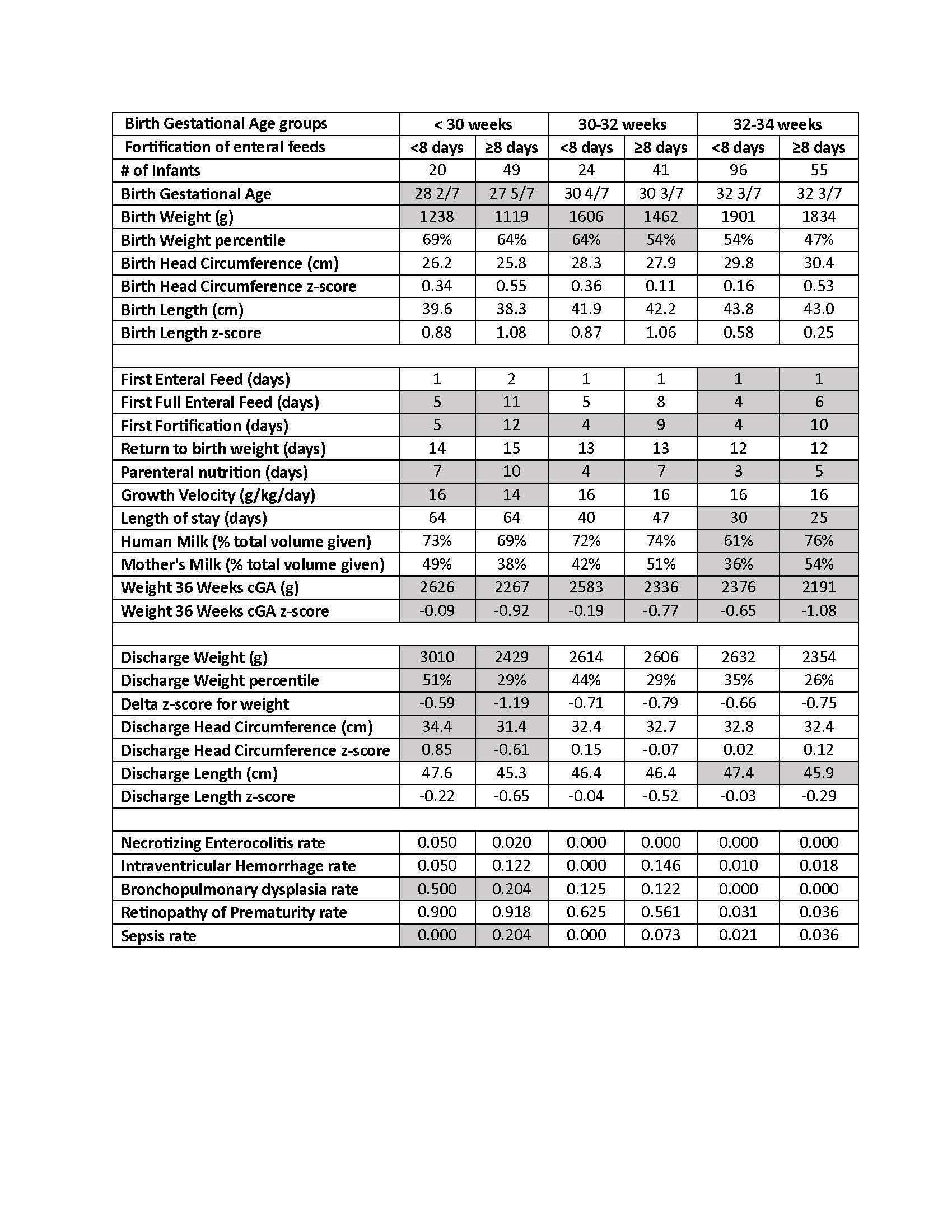
Results: A total of 362 preterm infants were included and divided into three cohorts, 2016-2018, 2019-2021, and 2022-2023. Feeding practices, growth parameters, and outcomes in both the 2016-2018 and the 2022-2023 cohorts were analyzed (Table 1). Birth growth parameters were similar between all periods. The day of first full enteral feed (120cc/kg/day) occurred significantly sooner as well as the day of first fortification with a subsequent decrease in parenteral nutrition (PN) use. Even though the days required to return to birth weight and the growth velocity did not significantly change, there was a significant increase in the delta z-score for weight, as well as the discharge z-scores for head circumference (HC) and length. Despite a significant reduction in the percentage of human (and maternal) total milk volume given during the hospitalization, there was a non-significant decrease in necrotizing enterocolitis and a significant decrease in sepsis rates. Then, study participants were divided by GA and by achievement of full feeds (Table 2) or fortification (Table 3) within the first week of life, and groups were compared. Infants fed earlier had a significant decrease in PN days, sepsis, and improved growth velocity in all groups, especially VLBW infants. Earlier fortification significantly impacted the weight z-score at 36wks corrected GA across all groups. Throughout the study period, length of stay significantly increased for infants < 32 weeks as well as a later first day of oral feeding.
Conclusion(s): Enteral feeding of preterm infants shortly after birth with faster volume advancement and early fortification should become the standard of care. This quasi-experimental study shows that these interventions improve all growth metrics (weight, HC and length) while decreasing the prevalence of sepsis.