Mental Health
Session: Mental Health 2
571 - Telepsychiatry Expansion of Inpatient Psychiatry Services on a Med/Surg Unit during the COVID-19 Pandemic
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 571
Publication Number: 571.1987
Publication Number: 571.1987

Nicole Penwill, MD, MPH (she/her/hers)
Assistant Professor, Section of Hospital Medicine
Children's Hospital Colorado
Denver, Colorado, United States
Presenting Author(s)
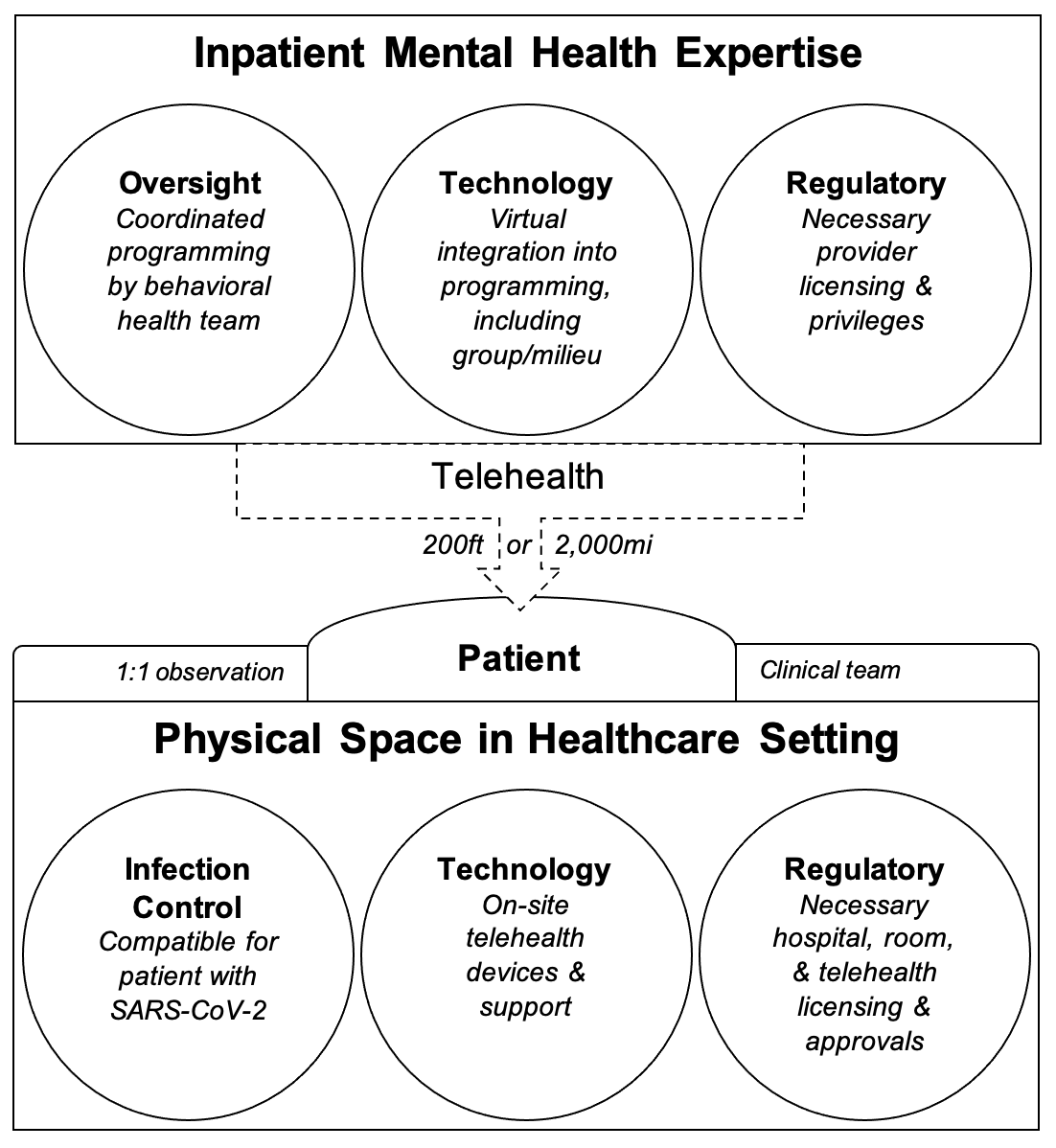
Background: During the COVID-19 pandemic, most psychiatric facilities could not admit youth with SARS-CoV-2 positivity, resulting in prolonged boarding times & delayed access to psychiatric services. Our children’s hospital enacted “IPU8” (Inpatient Psychiatry Unit 8th Floor), an innovative model allowing admission of SARS-CoV-2+ patients to ‘psych safer’ rooms on the inpatient medical unit with comprehensive telehealth psychiatric programming.
Objective: To evaluate the first 3 years of a novel inpatient telepsychiatry care model.
Design/Methods: To ensure safety and likelihood of clinical success, we defined IPU8 admission criteria as patients who required inpatient psychiatric care who were not aggressive, nonverbal, impulsive/hyperactive (unable to tolerate COVID-19 isolation precautions), or floridly manic or psychotic. We optimized environmental safety on the medical unit using pre-existing ‘psych safer’ rooms (mitigated ligature risk), removal of unsafe medical equipment, admission patient/belonging searches, and 1:1 continuous patient observation by a Behavioral Health Specialist. The psychiatrist was the admitting attending & primary clinical contact. A medical bedside nurse managed day-to-day care. Clinical managers from our inpatient psychiatric unit supervised daily psychiatric programming. While most psychiatric care was delivered via telehealth, some staff treated patients in-person with personal protective equipment after introduction of COVID-19 vaccination. IPU8 patients received the standard treatment protocol of our inpatient psychiatry unit including twice weekly family therapy and daily psychiatrist sessions, individual therapy, and milieu group therapy sessions. Pediatric hospitalists provided medical consultation on admission.
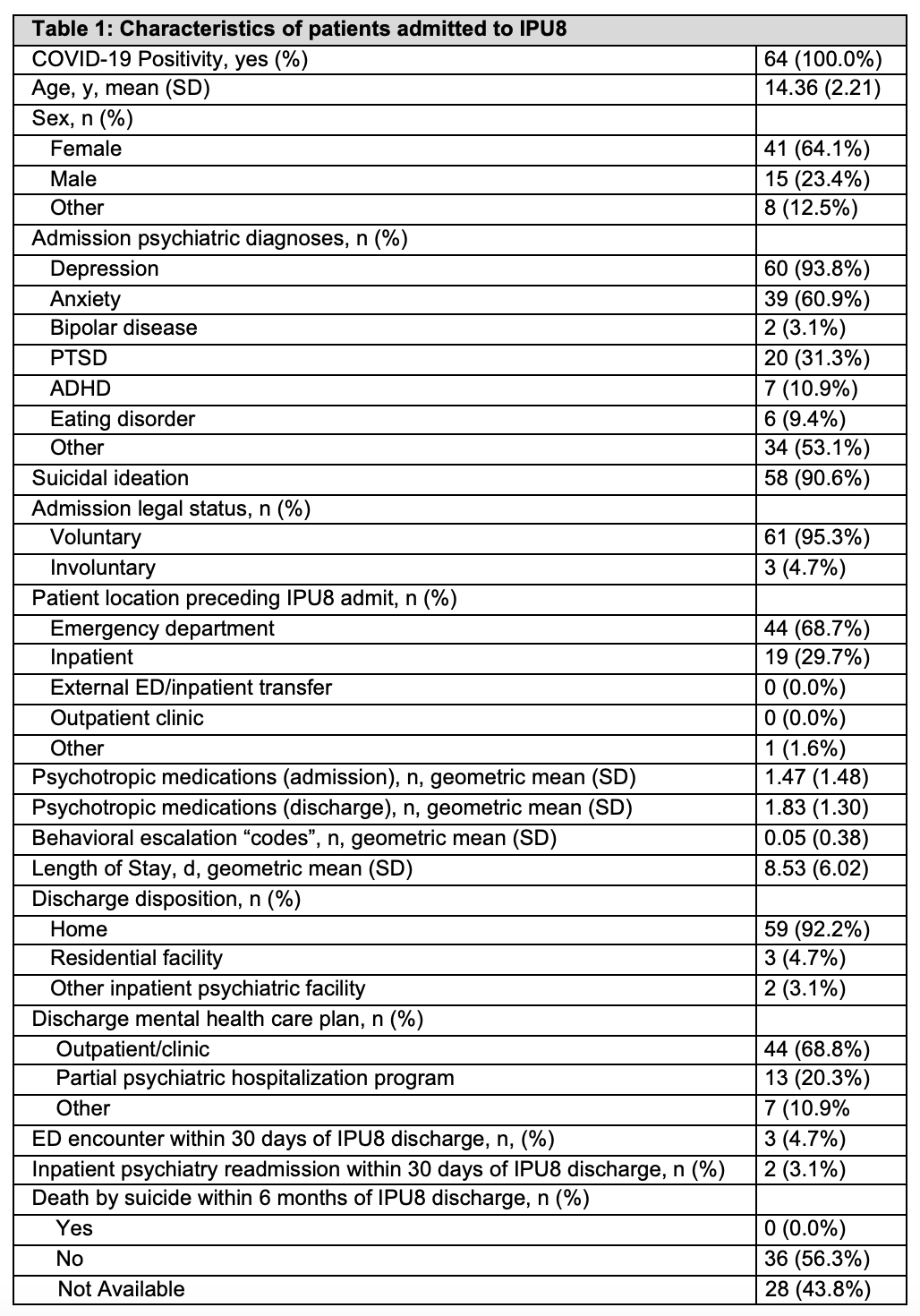
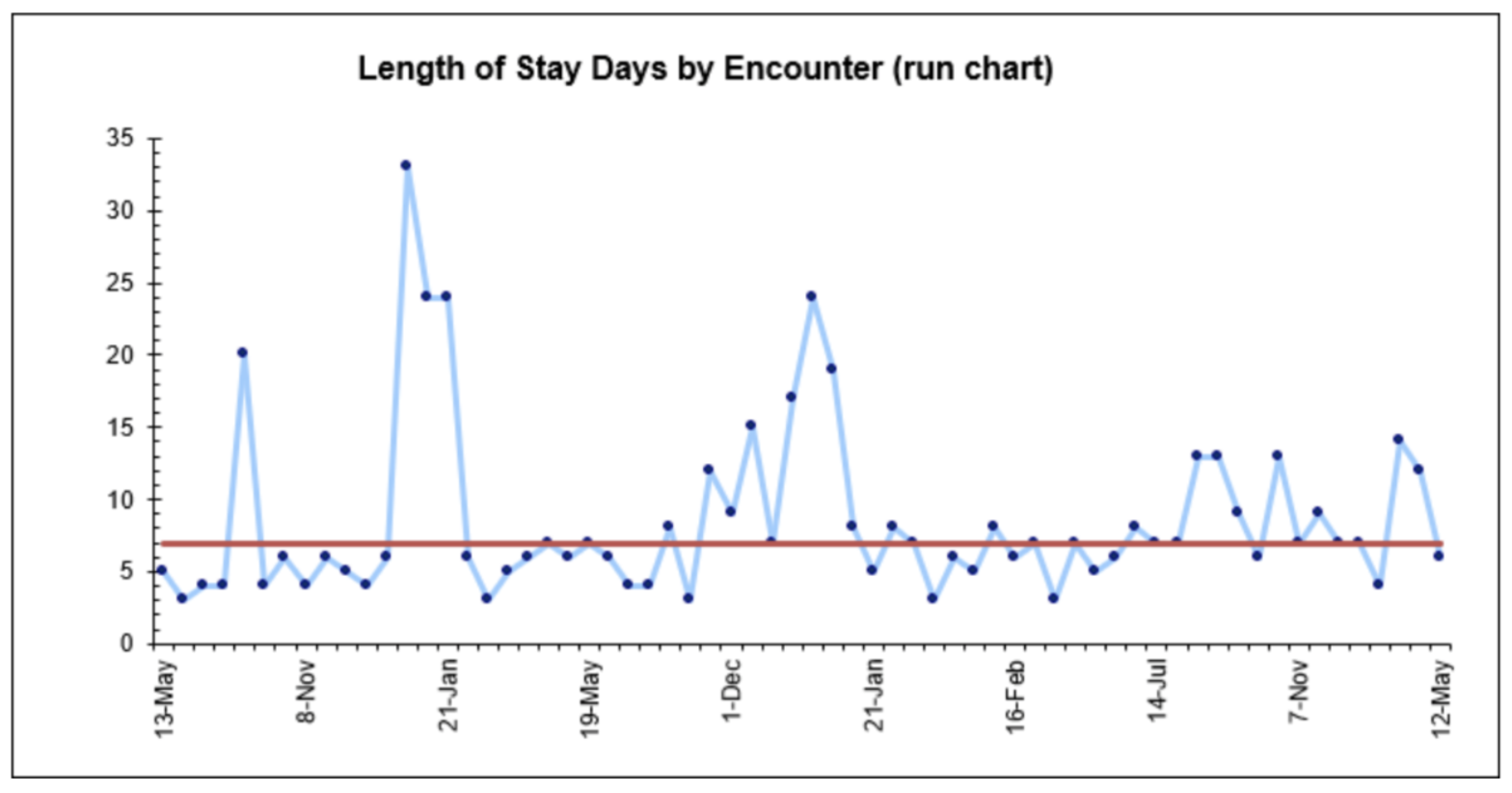
Results: Since May 2020, 64 SARS-CoV-2 positive pediatric patients have been admitted to IPU8 for treatment of their acute psychiatric condition(s) (Table 1). Less than 5% experienced ED or inpatient psychiatric readmission within 30 days of IPU8 discharge. No IPU8 patients died by suicide within 6 months of discharge (data available for 56.3% of patients).
Conclusion(s): We operationalized a novel model of inpatient-level psychiatric care for SARS-CoV-2+ youth experiencing mental health crisis using telehealth on our inpatient medical unit. This novel model of intensive mental health care has potential applications to future infectious outbreaks as well as to delivery of psychiatric services to patients with high medical complexity, during inpatient psychiatry capacity crises, and in geographic locations with limited access to inpatient pediatric psychiatric care.