Neonatology
Session: Neonatal GI Physiology & NEC 2: Enteral Nutrition and Growth
526 - Association between Diet and Fecal Calprotectin Levels in Very Preterm Infants
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 526
Publication Number: 526.1990
Publication Number: 526.1990

Jocelyn Ou, MD (she/her/hers)
Assistant Professor
Emory University School of Medicine
Atlanta, Georgia, United States
Presenting Author(s)
Background: Fecal calprotectin is a marker of intestinal inflammation and has been studied as a biomarker for diagnosing necrotizing enterocolitis (NEC) in preterm infants. Elevated levels may also occur in infants without NEC who present with feeding intolerance or bloody stools. Data on the effect of infant diet on fecal calprotectin levels are conflicting; some studies show no effect, while others show formula, cow’s milk fortifier or exclusive human milk feeding associated with higher fecal calprotectin levels.
Objective: We aim to determine the association between diet (maternal human milk, donor human milk, or formula) and fecal calprotectin in very preterm infants.
Design/Methods: We performed a secondary analysis of a prospective birth cohort study of infants with a birth weight ≤ 1250 g and gestational age < 33 weeks. Stool samples were collected weekly and fecal calprotectin was measured by enzyme linked immunosorbent assay. Diet information was recorded daily (maternal breast milk, donor breast milk, or formula). We analyzed diet 0-3, 3-6, 6-9, and 9-12 days before calprotectin measurement. Associations between infant- and feeding-related characteristics and calprotectin were then assessed using mixed-effects regression models, accounting for within-infant correlation and confounding variables.
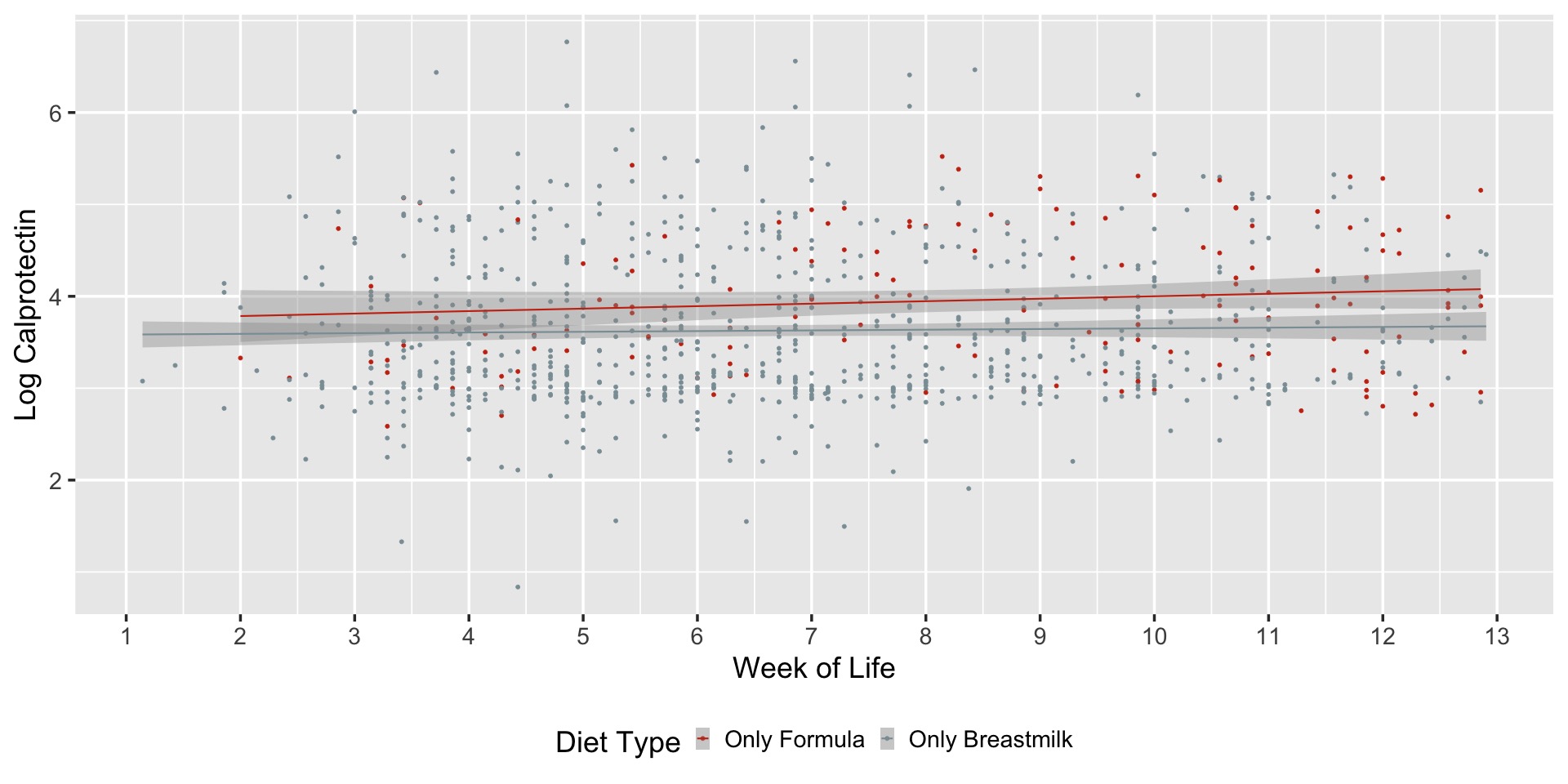
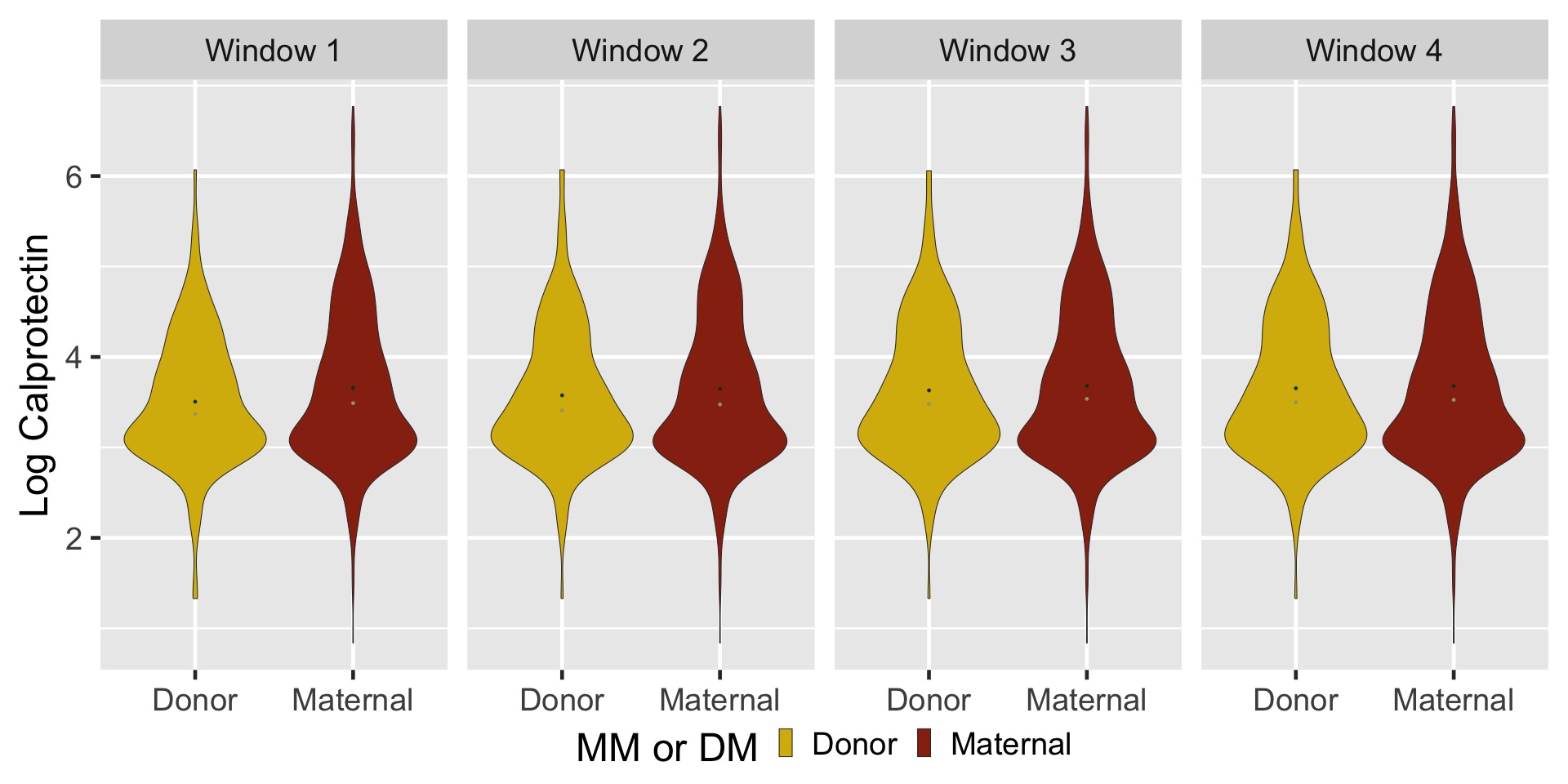
Results: We analyzed 227 infants with available feeding data (17,016 daily feeding observations and 1704 calprotectin measurements). Infants fed human milk had lower fecal calprotectin levels compared with those fed cow’s milk formula for 0-3, 3-6, and 6-9 day windows (all p < 0.05). Infants receiving full feeds (defined as >80% of total) of only human milk had lower log calprotectin levels than those receiving only formula (-0.35; 95% CI -0.52, -0.17; P< 0.001 at 0-3 days, with similar estimates at 3-6 and 6-9 days prior to calprotectin measurement. The mean difference in calprotectin was small when considering the variability of measures over postnatal age (Figure 1). There was no difference in fecal calprotectin between donor and maternal milk.
Conclusion(s): Infants fed formula compared to breast milk have higher fecal calprotectin levels. Although diet is associated with fecal calprotectin, feeding measures only explain a small amount of the variability of calprotectin in very preterm infants.