Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 6
52 - Pilot Implementation of a Health-Related Social Needs Screen in a Hospital-based Pediatric Cardiology Clinic
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 52
Publication Number: 52.2936
Publication Number: 52.2936

Karina Javalkar, MD (she/her/hers)
Pediatric Cardiology Fellow
Boston Children's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Social determinants of health impact health outcomes in patients with congenital heart disease (CHD), with fewer resources and lower socioeconomic status linked to adverse cardiac outcomes.
Objective: The aims of this QI project were to evaluate the feasibility of implementing a health-related social needs (HRSN) screener in a busy cardiology clinic, and identifying and responding to patients’ needs.
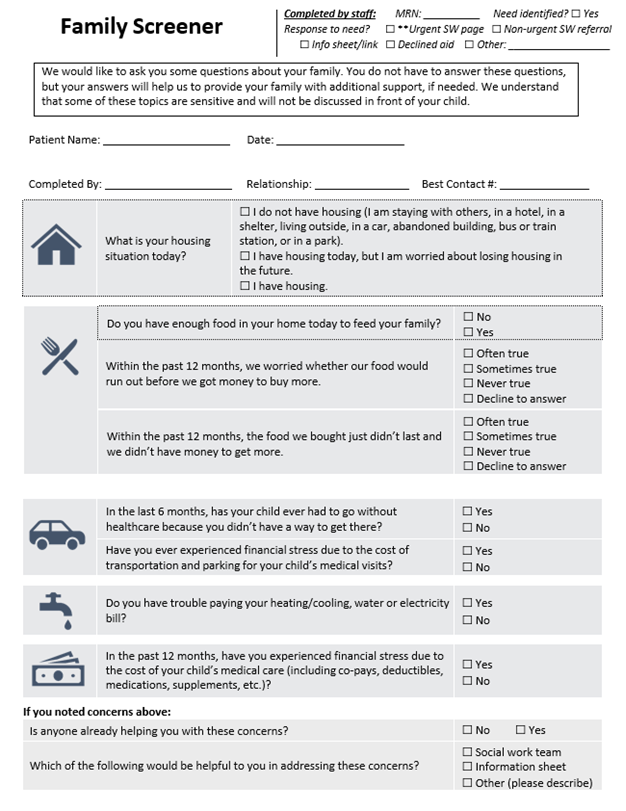
Design/Methods: We developed a HRSN screening tool by adapting nationally and locally validated tools (Figure 1). We designed a workflow for distributing the tool, evaluating responses, and providing need-specific information (handout or web link) and social work (SW) referrals when appropriate. The process was revised in multiple iterations based on feedback, including rearranging questions and answers, multi-language translation, and improving resource distribution including with QR links. Weekly stakeholder meetings evaluated impact of implementation on clinic flow. Process measures included stakeholder feedback and number of screeners completed. Outcome measures included the number of needs identified and SW referrals. Balancing measures included time spent by the clinician and SW team.
Results: We implemented the tool incrementally to increasing numbers of clinicians (initially 3 fellows, now up to 7 fellows and 7 attendings) over the course of 4 months. The pilot included 77 completed screeners, with 20 (26%) identifying at least one need among assessed domains; 13 (17%) identified a need in >1 domain. Urgent in-clinic SW input was needed for 5 (6%) for no food or housing that day. SW provided a follow up phone call in 10 (13%). Resources distributed included information sheets/links (2 patients), parking vouchers (3), transportation (1), and grocery cards (1). SW feedback noted more families with needs have been identified compared to prior to screening implementation; volume is manageable with current SW resourcing. Of the 12 families desiring SW intervention, SW spent a median of 45 min/patient (range 15-120 minutes). Multidisciplinary provider buy-in as well as feedback to the screener were positive.
Conclusion(s): Implementing a HRSN screener is feasible within a busy cardiology clinic and facilitated distribution of resources to patients with minimal modification to clinic workflow. Outpatient SW plays a crucial role in ambulatory pediatric cardiology care; additional SW resources will be needed when scaled to all providers. Investment from providers around the importance of HRSN evaluation in patients with CHD is essential to improve outcomes.