Emergency Medicine
Session: Emergency Medicine 6: Airway and POCUS
200 - Spinal Anatomy Ultrasound in Young Infants with Implications for Lumbar Puncture
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 200
Publication Number: 200.1709
Publication Number: 200.1709

Margaret Barton Barton, MD (she/her/hers)
Fellow in Pediatric Emergency Medicine
Monroe Carell Jr. Children's Hospital at Vanderbilt
Nashville, Tennessee, United States
Presenting Author(s)
Background: Clinicians may struggle to obtain cerebral spinous fluid (CSF) during young infant lumbar punctures (LPs) as it can be difficult to feel the needle pass through structures and the amount of available CSF is uncertain. Successful LPs in infants might be maximized by accurate understanding of patient anatomy, including optimal site and depth of needle insertion using ultrasound (US).
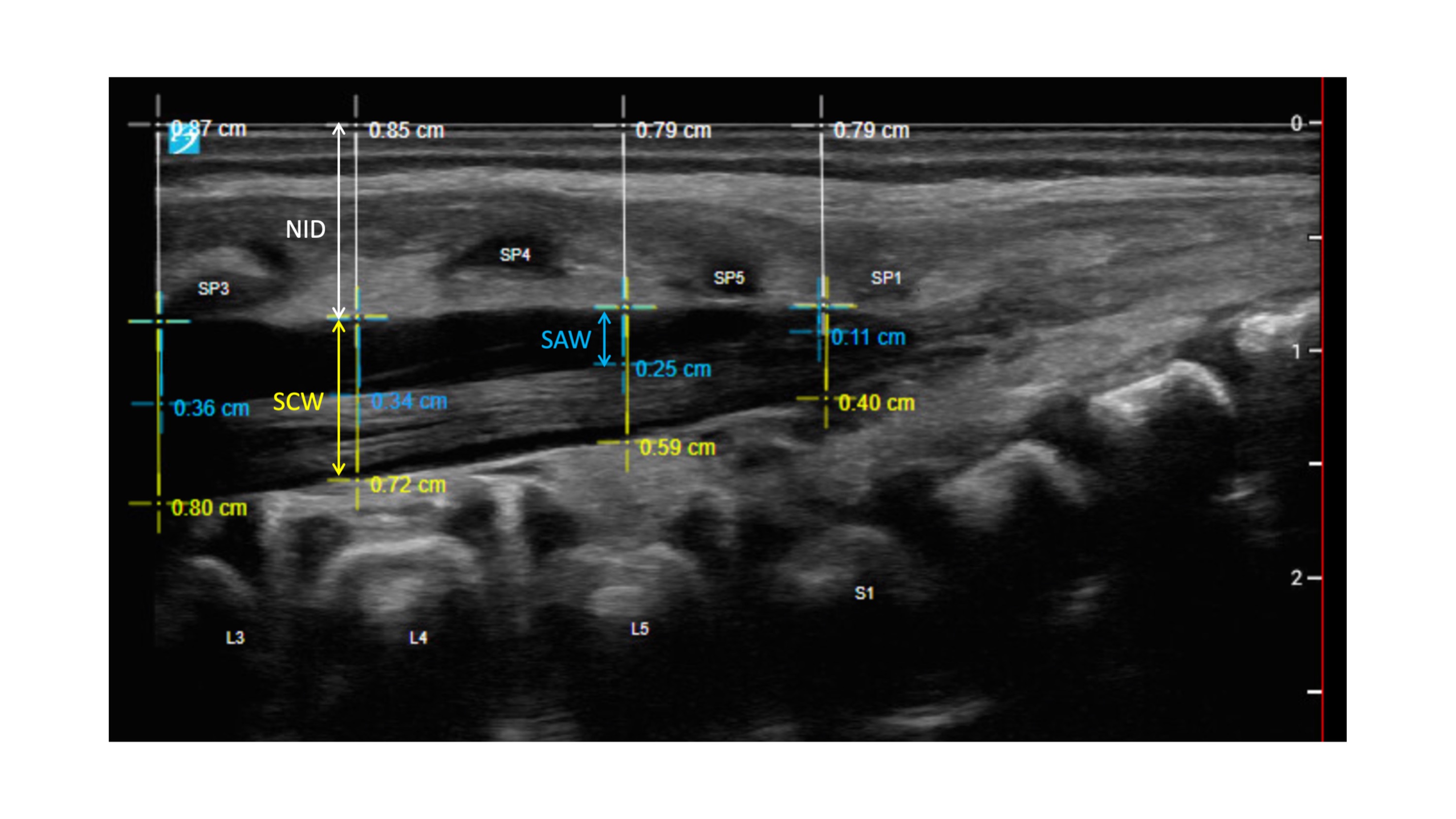
Objective: 1) Determine the optimal site of lumbar puncture in young infants by examining spinal anatomy with US at L2/L3-L5/S1 to determine differences in needle insertion depth (NID), spinal canal width (SCW), and subarachnoid fluid width (SAW).
2) Predict NID of L2/L3-L5/S1 in young infants based on variables including age, gestational age, height, and weight.
Design/Methods: We studied a convenience sample of participants aged 0-6 months in a tertiary children’s Emergency Department. Exclusion criteria included known spinal pathology, prior LP within twenty-four hours, and severe illness. We recorded characteristic data including age, gestational age at birth, gender, race, height, weight, and hydration status. We used a Sonosite PX US with a linear 15 MHz transducer to image each participant’s spine in the left lateral decubitus position. Landmarks were confirmed using the lumbo-sacral junction. Images were reviewed on Q-path. We used the paired t-test to examine univariate differences in NID, SCW, and SAW. Multiple linear regression models were used to derive predictive equations for NID.
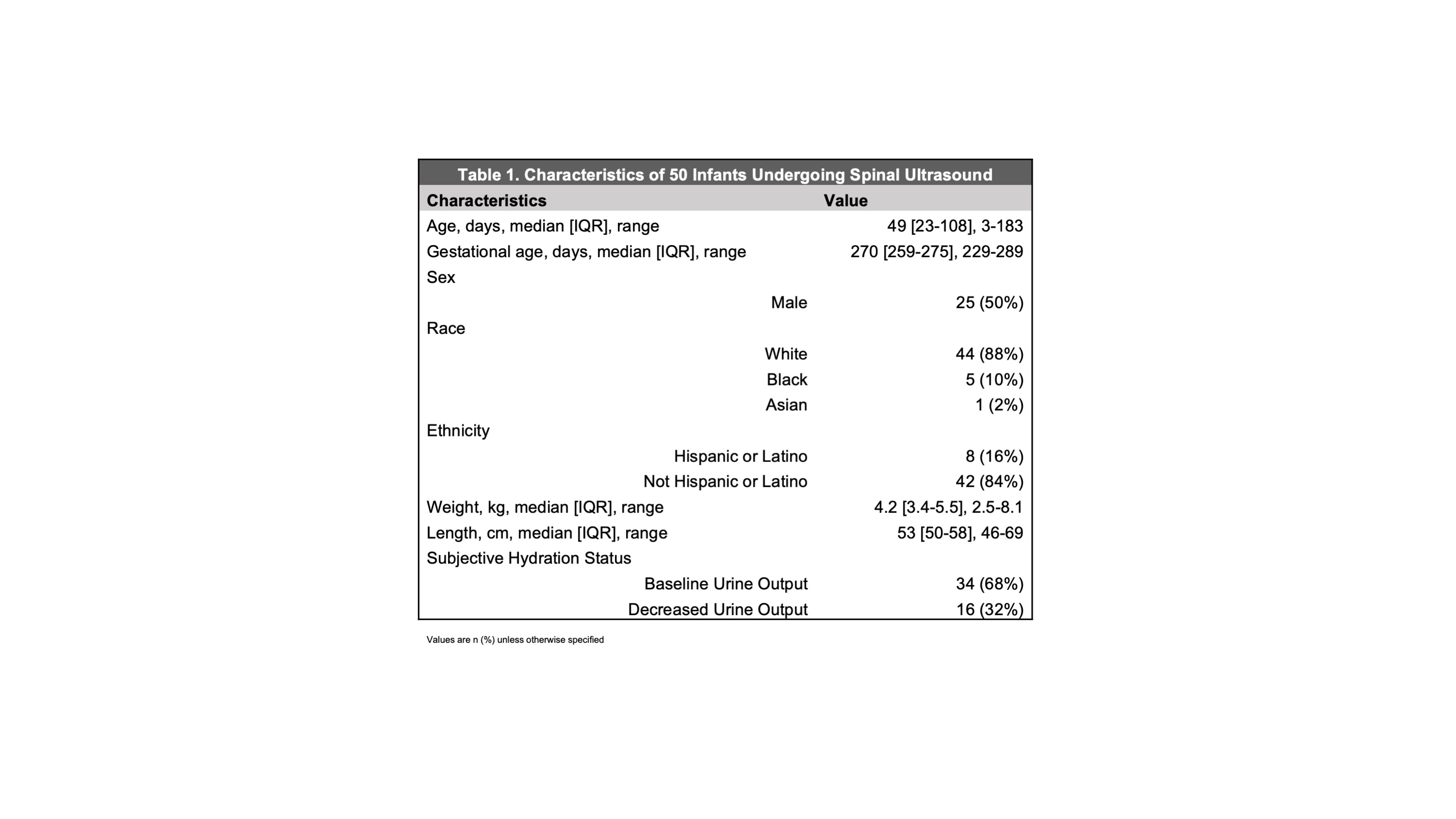
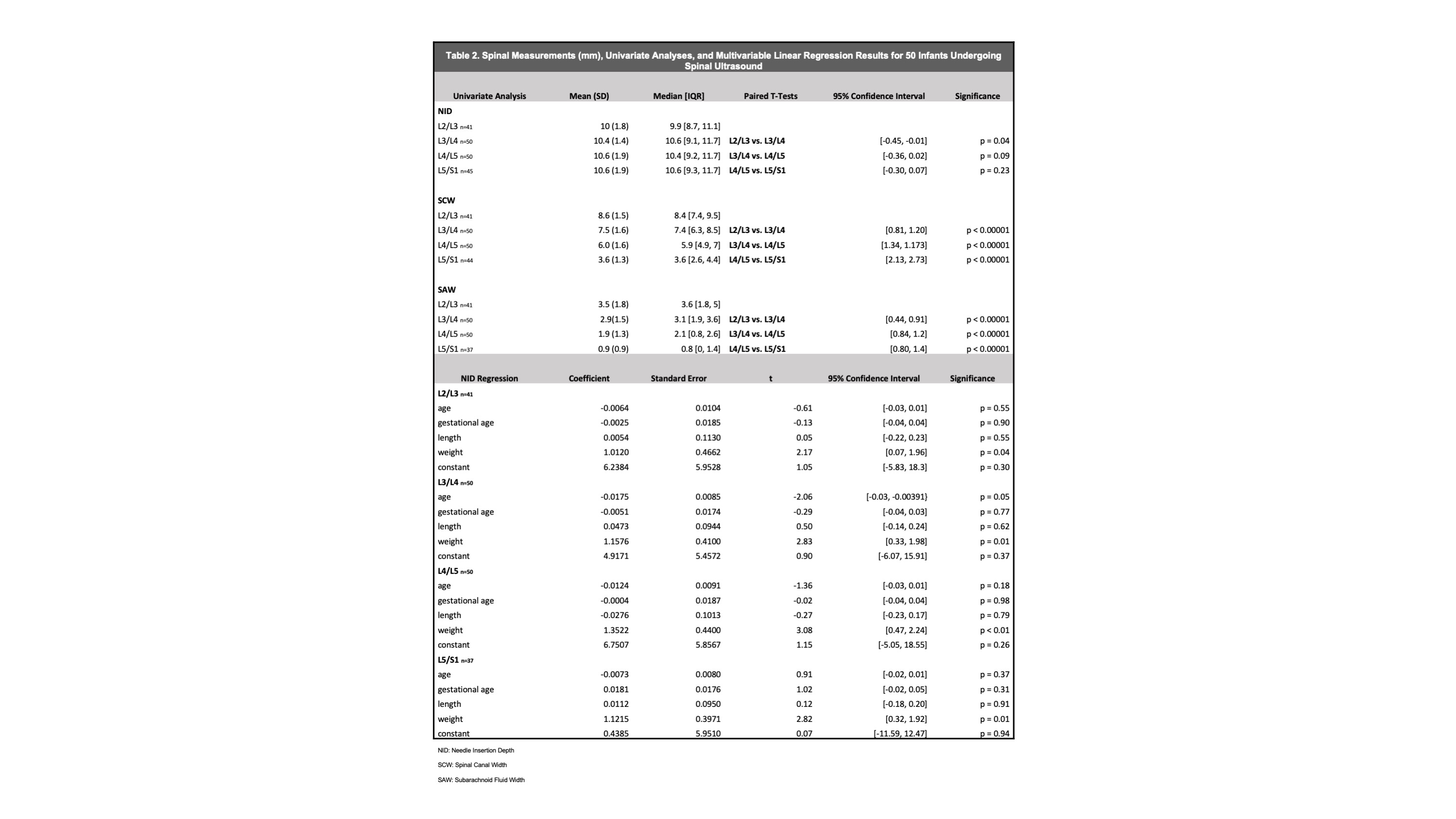
Results: Participant characteristics are displayed in Table 1. Measurements and differences in NID, SCW, and SAW are shown in Table 2. Weight was associated with NID after adjusting for other covariates in a multivariable linear regression model.
Conclusion(s): Spinal canal width and subarachnoid fluid width are consistently measured to be larger the more cephalad the site, suggesting success may be maximized at higher intervertebral spaces. Subarachnoid fluid width was consistently measured to be small. Therefore, it is important to use precise movements when near the target CSF. Location of the needle site does not markedly change expected needle depth which was approximately 1 centimeter across all sites (with differences in tenths of millimeters). Weight can be used to estimate optimal needle insertion depth unlike age, gestational age, and length; although, it is unclear whether such small differences of depth would make a clinical difference.