Emergency Medicine
Session: Emergency Medicine 8: Mental Health
581 - Impact of the COVID-19 Pandemic on Demographic and Clinical Trends in Pediatric Intentional Self-Poisonings
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 581
Publication Number: 581.1717
Publication Number: 581.1717
Hannah Wilkins, MD
Assistant Professor
University of Arkansas for Medical Sciences College of Medicine
Little Rock, Arkansas, United States
Presenting Author(s)
Background: The COVID-19 pandemic has devastated the mental health of children and adolescents, resulting in more hospital admissions for suicidality and self-harm including deliberate self-poisonings. No prior studies report and compare detailed demographic and clinical data on pediatric intentional ingestions before and during the pandemic utilizing a national registry.
Objective: This study aims to compare demographics, clinical characteristics, management, and outcome data of pediatric patients with intentional self-poisonings before and during the COVID-19 pandemic.
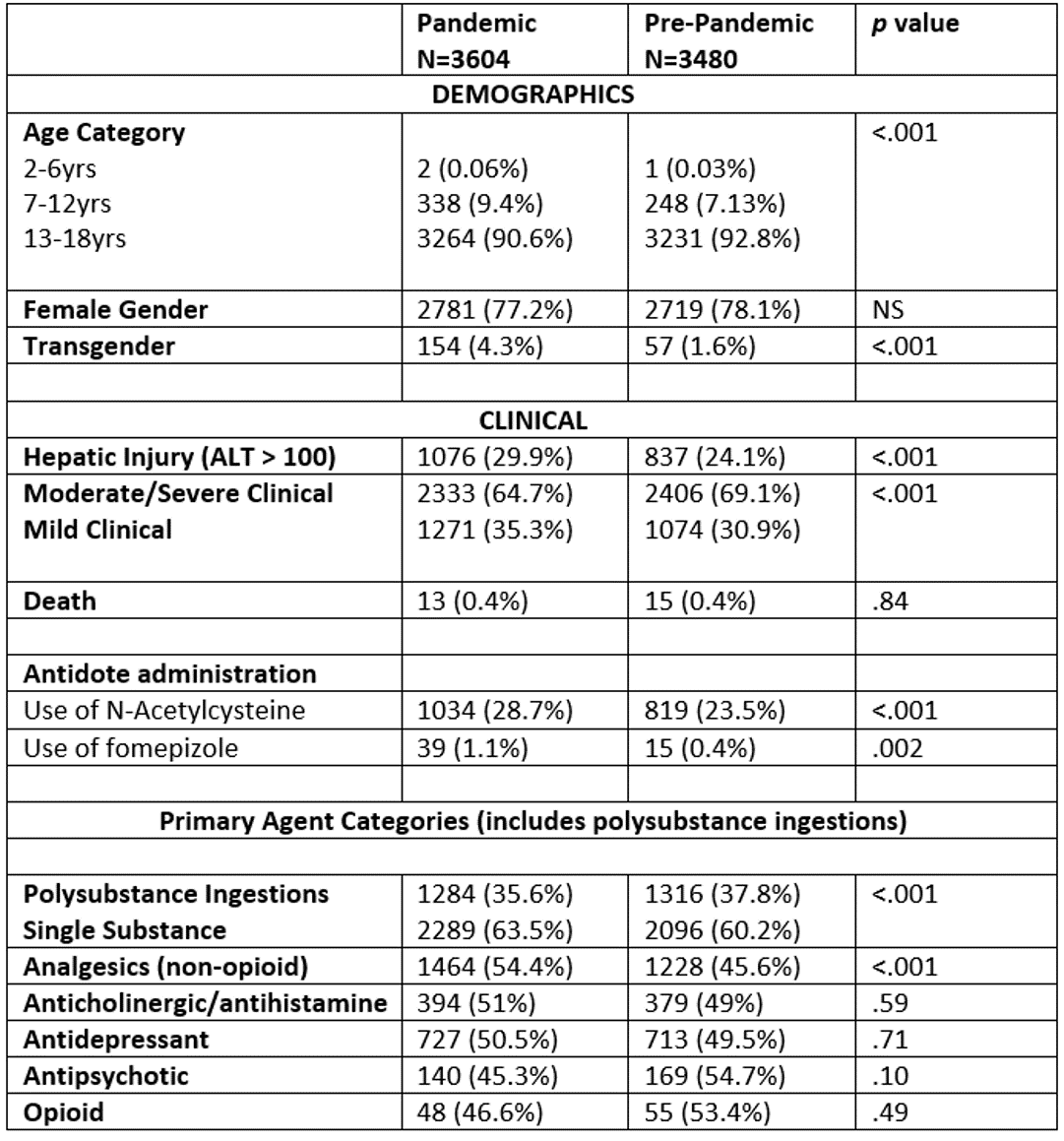
Design/Methods: We retrospectively reviewed de-identified data from the Toxicology Investigators’ Consortium registry of all patients ages 6-18 years presenting with intentional self-poisoning, whether self-harm or deliberate misuse. All cases were reported by medical toxicologists evaluating these patients at participating sites. The study period was divided into Pre-Pandemic April 2017-February 2020 (PreP) and Pandemic March 2020-October 2022 (PAND). Moderate/severe outcome was defined as those patients who received critical care treatment or died. Chi-square analyses and Fisher’s exact test were performed to determine associations among variables between the PreP and PAND periods, with p value < 0.05 being significant. SAS 9.4 (SAS Institute, Cary, NC) was used to perform statistical analyses.
Results: 7,084 cases met inclusion criteria: 3,480 PreP and 3,604 PAND. The PAND cohort had a higher percentage of cases in the 7-12 year age group, patients identifying as transgender, and non-opioid analgesics as a primary agent (see Table). During the pandemic, the odds of intentional self-poisoning were greater in Asians (OR 1.47, 95% CI 1.05-2.04) and Black/African Americans (OR 1.19, 95% CI 1.03-1.38) compared to non-Hispanic Whites (p=.023 and .021 respectively). Conversely, non-Hispanic Whites had higher odds of pandemic self-poisoning than Hispanics (OR 1.29, 95% CI 1.12-1.49, p<.001). There was a greater frequency of moderate/severe outcomes in the PreP cohort with more polysubstance ingestion, anticholinergic toxidrome, tachycardia, ECG abnormalities, and CNS depression. The PAND group required more fomepizole and N-acetylcysteine therapy for toxic alcohol and acetaminophen respectively. There was no difference in mortality or use of vasopressors, cardioversion, CPR, or ECMO.
Conclusion(s): The age, gender, and ethnicity differences suggest a disparate impact of the pandemic on these vulnerable populations. The full effect of the pandemic remains to be seen.