Neonatology
Session: Neonatal Neurology 1: Clinical
2 - Genetic and Congenital Anomalies in Newborns with Hypoxic-Ischemic Encephalopathy
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 2
Publication Number: 2.141
Publication Number: 2.141

Adriana S. Morell, MD (she/her/hers)
Assistant clinical professor
University of California, San Francisco, School of Medicine
San Francisco, California, United States
Presenting Author(s)
Background: Infants diagnosed with HIE may have underlying conditions predisposing them to sustaining hypoxic-ischemic injury during the labor and delivery process. It remains unclear how the presence of a genetic or congenital anomaly impacts the clinical presentation and outcomes of HIE.
Objective: We determined the frequency of diagnosed and unsuspected genetic or congenital anomalies in infants with HIE, and whether such anomalies are associated with severity of encephalopathy or with neurodevelopmental outcomes.
Design/Methods: Infants with moderate or severe HIE enrolled in the HEAL trial underwent genetic testing when clinically indicated (e.g., dysmorphic features, family history, organ anomaly). Congenital anomalies, defined as structural malformation of a major organ system, were diagnosed prior to hospital discharge, and were prospectively recorded. The primary outcome, i.e., death or neurodevelopmental impairment (NDI), was determined at 22-36 months of age by a standardized neurologic examination, Bayley Scales of Infant Development-III (BSID-III), and the Gross Motor Function Classification Scales. Secondary outcomes included cerebral palsy, 5-level ordinal outcome (no NDI, mild NDI, moderate NDI, moderate NDI, severe NDI, or death), gross motor function classification system (GMFCS) >= 1 and BSID-III motor, cognitive and language scores at age 22-36 months.
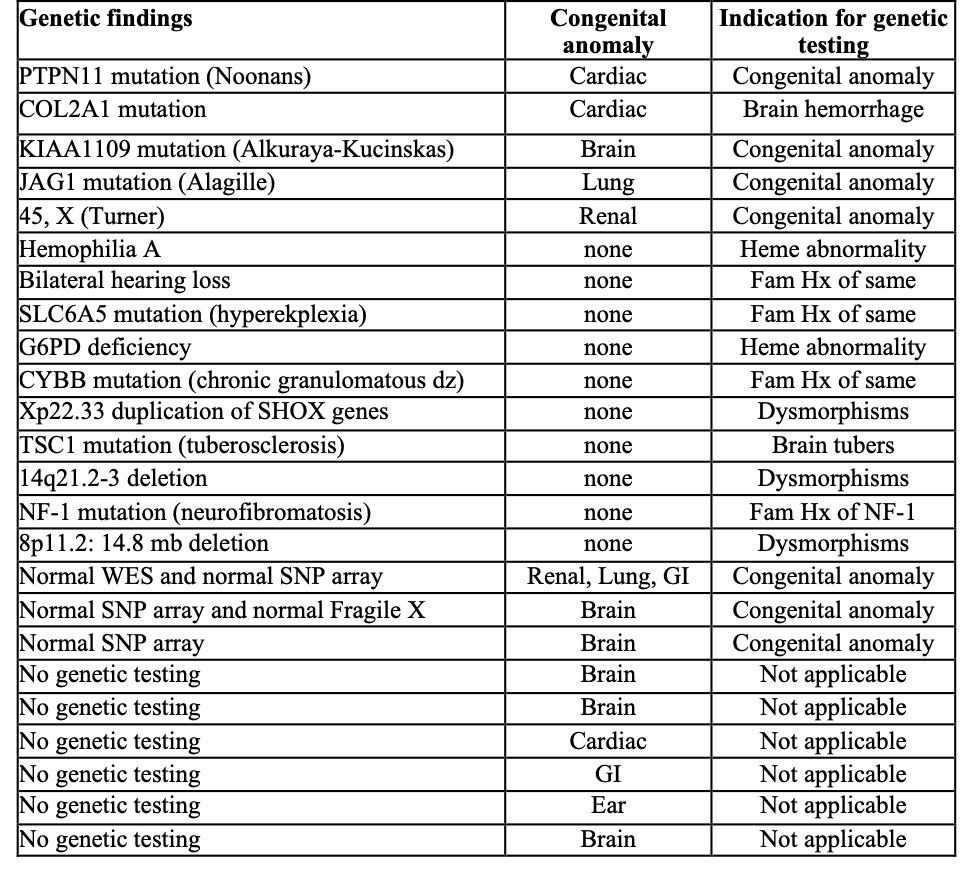
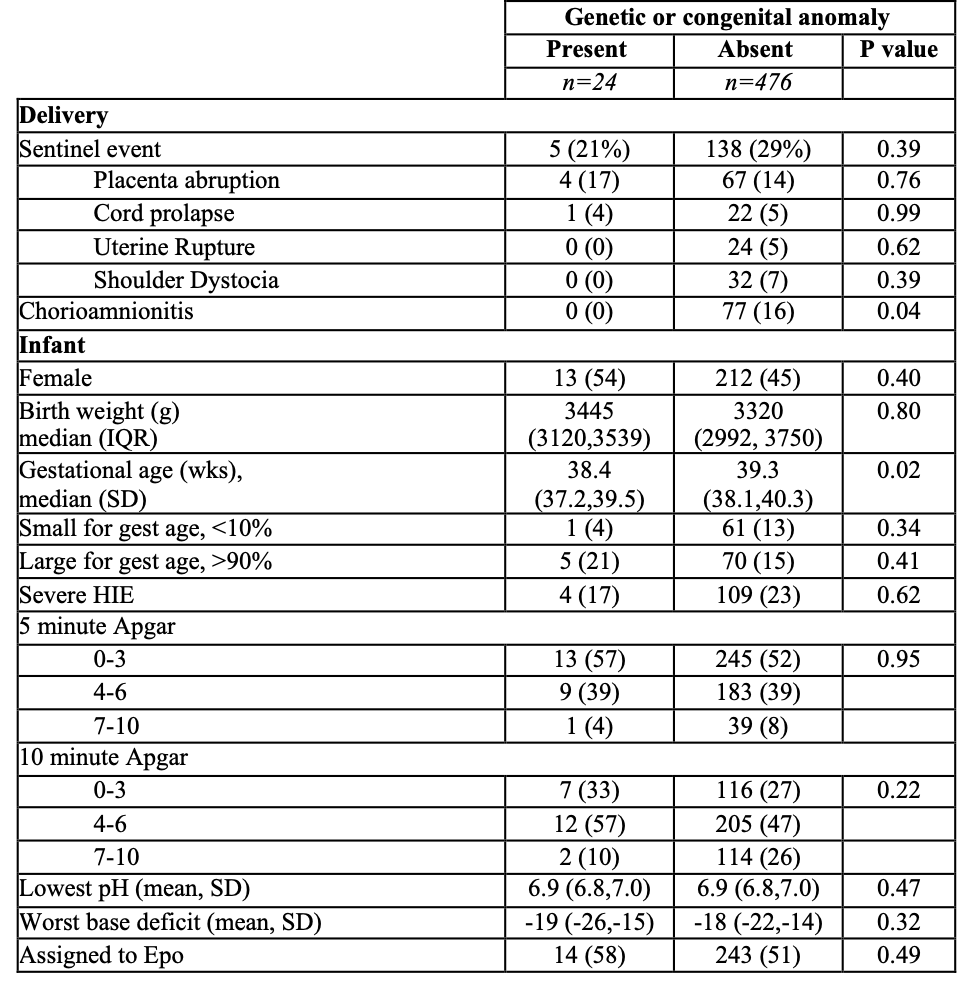
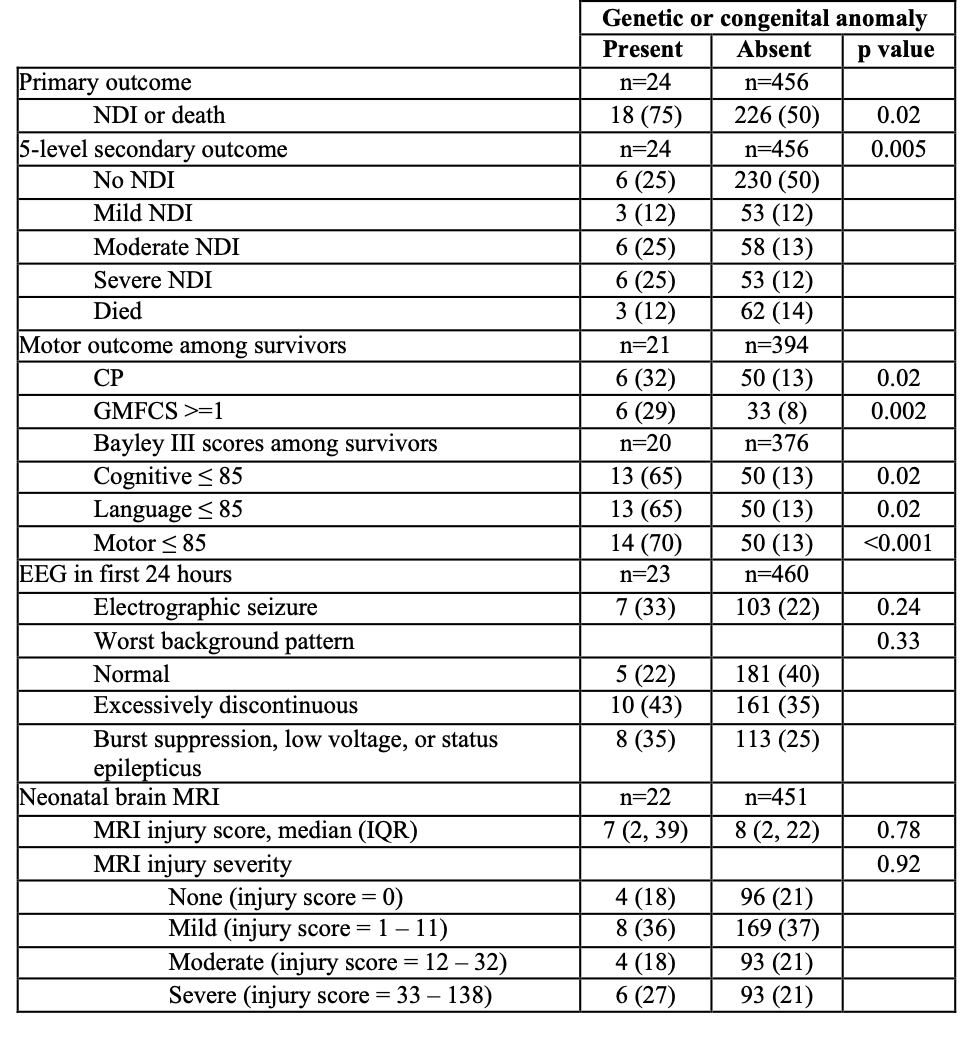
Results: Of 500 infants with HIE, 24 (5%, 95% CI 3-7%) were diagnosed with a genetic or congenital anomaly, including 10 (2%) with only a genetic anomaly, 9 (2%) with only a congenital anomaly, and 5 (1%) with both (Table 1). Infants with and without genetic or congenital anomalies had similar rates of severe encephalopathy (17% vs. 23%, P=0.62) (Table 2) and similar findings on neonatal EEG and brain MRI (Table 3). However, infants with genetic or congenital anomalies were more likely to have the primary outcome of death or NDI (75% vs 50%, P= 0.02) (Table 3). Among survivors, those with a genetic or congenital anomaly were more likely to be diagnosed with cerebral palsy (32% vs. 13%, P =0.02), and more likely to have a low (<=85) BSID-III score in cognitive (65% vs. 13%, P=0.02), language (65% vs 13%, P=0.02) and motor (70% vs 13%, P= < 0.001) domains than HIE survivors without such anomalies (Table 3).
Conclusion(s): Among infants with HIE the frequency of diagnosed genetic or congenital anomalies was 5%. Despite similar clinical markers of HIE severity, infants with HIE and a genetic or congenital anomaly had worse neurodevelopmental outcomes than infants with HIE alone.