Health Services Research
Session: Health Services Research 2: Novel Methods and Disparities
296 - Identifying Parents Who Feel Isolated Amongst the Isolettes: Lessons Learned from Routine Perinatal Mental Health Screening in a Neonatal Intensive Care Unit
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 296
Publication Number: 296.1494
Publication Number: 296.1494

Sarah A. Swenson, MD, DPhil (she/her/hers)
Neonatal-Perinatal Medicine Fellow
University of Minnesota Medical School
Minneapolis, Minnesota, United States
Presenting Author(s)
Background: The American Academy of Pediatrics neonatal standards of care include depression screening. Gaps remain regarding optimal screening practices. We implemented mental health (MH) screening for parents in a Level IV neonatal intensive care unit (NICU) as part of a quality improvement project.
Objective: Determine effect of routine NICU parent MH screening on detection of MH concerns
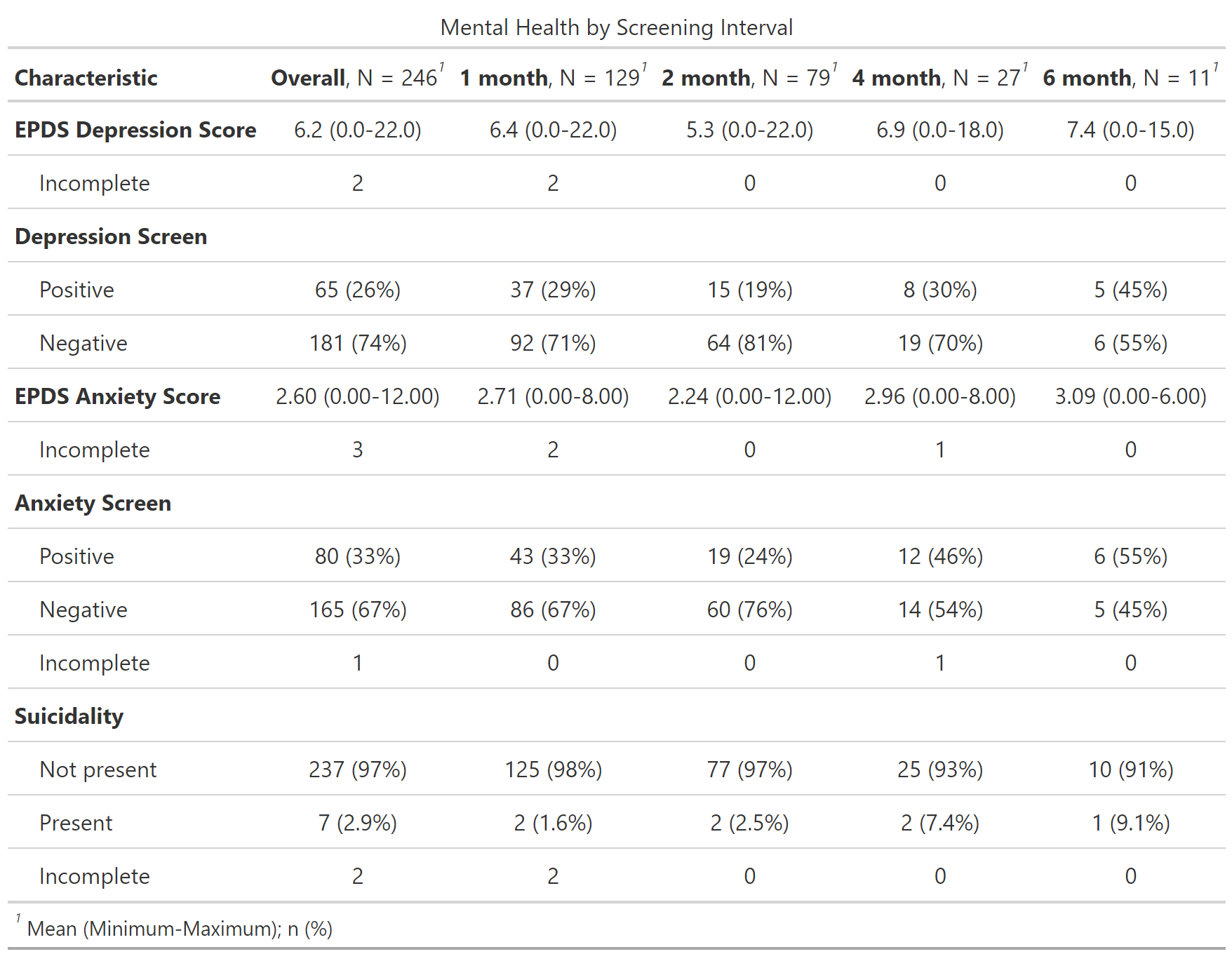
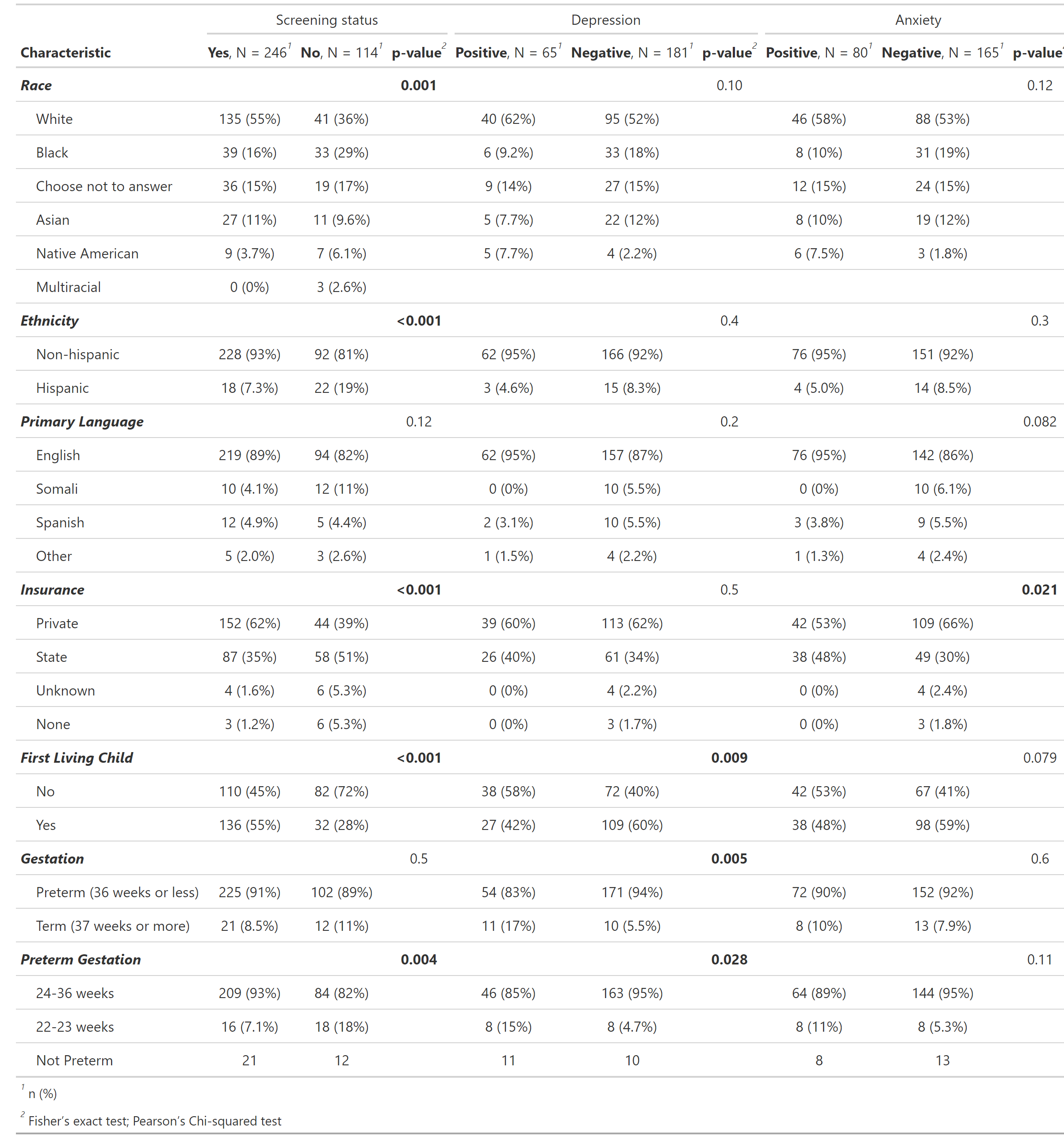
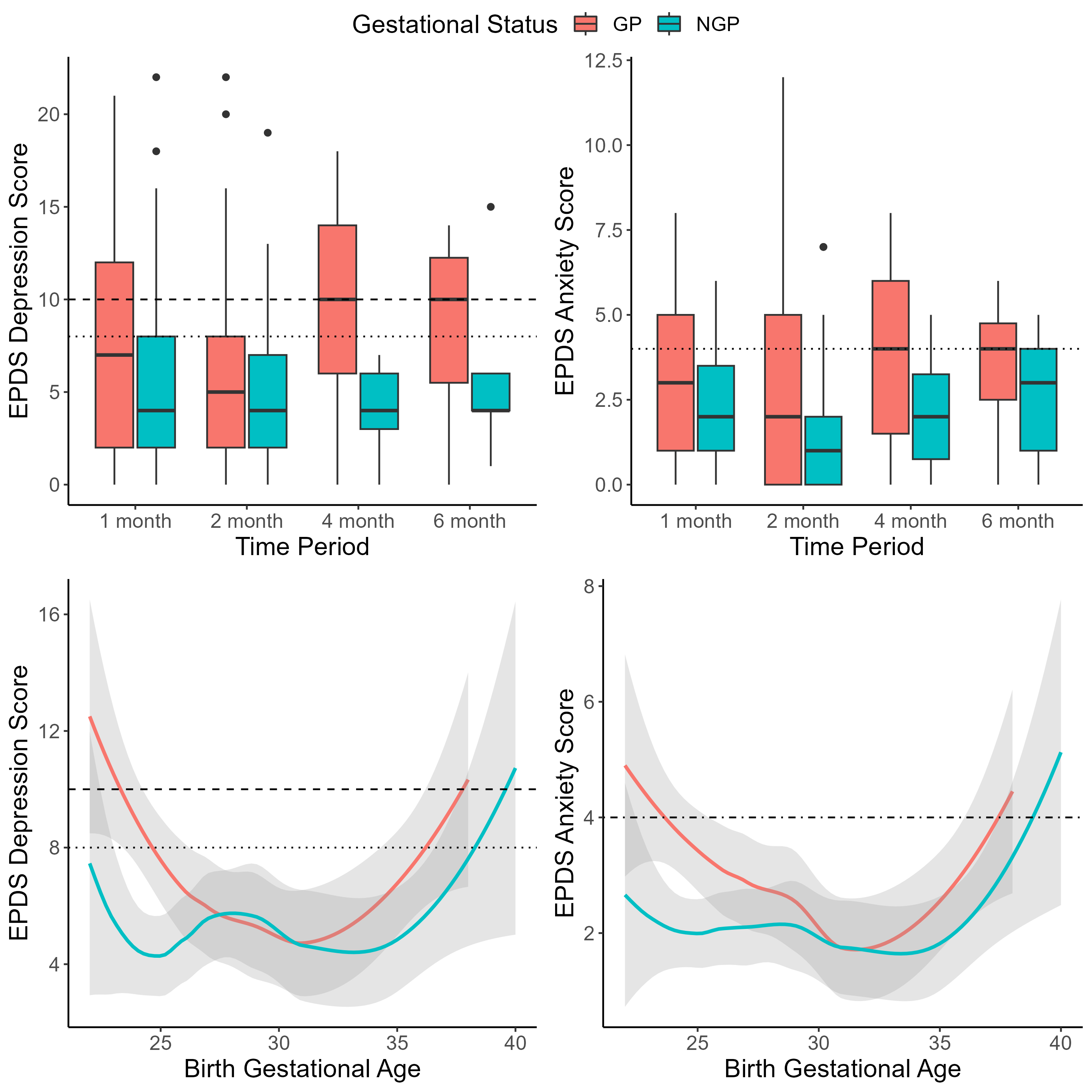
Design/Methods: MH concerns based on clinical interactions were tracked from March-September 2022. Social workers screened parents in the NICU at 1, 2, 4 and 6 months using the Edinburgh Postpartum Depression Scale (EPDS, threshold of 10 for gestational parents (GP) and 8 for nongestational parents (NGP)) and anxiety subscale (EPDS-3A, threshold of 4) from October 2022-August 2023. Characteristics and results were recorded. Descriptive counts and means were calculated and stratified. Average EPDS, EPDS-3A scores, and proportion of parents above thresholds were calculated by interval. Differences in key variables were assessed using Fisher’s exact and Pearson’s chi-square tests.
Results: Prior to screening, 59 parents were referred (56 GP, 3 NGP) with 71% occurring within 2 weeks of birth. In the screening period, 246 (138 GP, 108 NGP) of 340 eligible parents were screened. 65 EPDS were positive (43 GP (31%), 22 NGP (20%)). 80 EPDS-3A were positive (56 GP (41%), 24 NGP (22%)). 7 parents had suicidal ideation (4 GP (3%), 3 NGP (3%)). Parents at 6 months had the highest percent positive on EPDS (45%), EPDS-3A (55%), and suicidal ideation (9%) compared to other intervals. There were statistically significant differences in race (p=0.001), ethnicity (p < 0.001), insurance type (p < 0.001), and first living child (p < 0.001) between the screened and not screened groups. A higher proportion of parents with previous children (p=0.009), term infants (p=0.005), and preterm infants < 24 weeks (p=0.028) were positive on EPDS. There were significant differences in EPDS-3A positive rates between insurance types (p=0.021).
Conclusion(s): Few NGP with MH concerns were recognized prior to screening, and the percent of parents above screen threshold is highest at 6 months, affirming the need for inclusive screening at routine intervals. Depression screening alone may be inadequate. Populations who may benefit from targeted interventions given particular high risk of MH symptoms include parents with previous children, state insurance, term infants, and preterm infants < 24 weeks. Further interventions are needed to ensure equity and decrease barriers to receiving support. Results may be affected by parents appearing in the dataset more than once.