Breastfeeding/Human Milk
Session: Breastfeeding/Human Milk 3: Milk Composition
493 - Influence of Social Determinants of Health on Maternal Breastmilk Composition and Neonatal Growth for Infants Admitted to the Neonatal Intensive Care Unit
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 493
Publication Number: 493.1867
Publication Number: 493.1867

Ellen Ribar, MD (she/her/hers)
Resident
University of Colorado School of Medicine
Denver, Colorado, United States
Presenting Author(s)
Background: Preterm infants have high nutritional needs and are at risk for extrauterine growth failure. Although maternal breast milk (MBM) is the best source of nutrition for preterm infants, MBM composition, including macronutrient (carbohydrate, protein, and fat) and energy content, can vary widely. How maternal social determinants of health (SDH) impact milk composition has not been studied, but SDH are known to impact birth outcomes and maternal nutrition.
Objective: This study aims to evaluate how SDH may impact MBM composition. We hypothesize MBM from those with public insurance and who reside in a zip code with a median income below the state average will have lower energy and macronutrient content than MBM from those with private insurance and who reside in a zip code with a median income above the state average.
Design/Methods: This retrospective chart review at a single tertiary care children’s hospital in a level IV neonatal intensive care unit included infants < 2200 grams who were older than one week of age, receiving MBM, and not meeting predefined growth goals. Infants with cyanotic congenital heart disease and intestinal abnormalities were excluded. MBM caloric density and macronutrient content were quantified using an FDA approved human milk analyzer. Demographic information was abstracted from the electronic medical record. Data was analyzed using GraphPad Prism with unpaired t-tests or Mann Whitney tests for non-normally distributed data and linear regressions. P value of < 0.05 was considered statistically significant. Values indicate means ± SD.
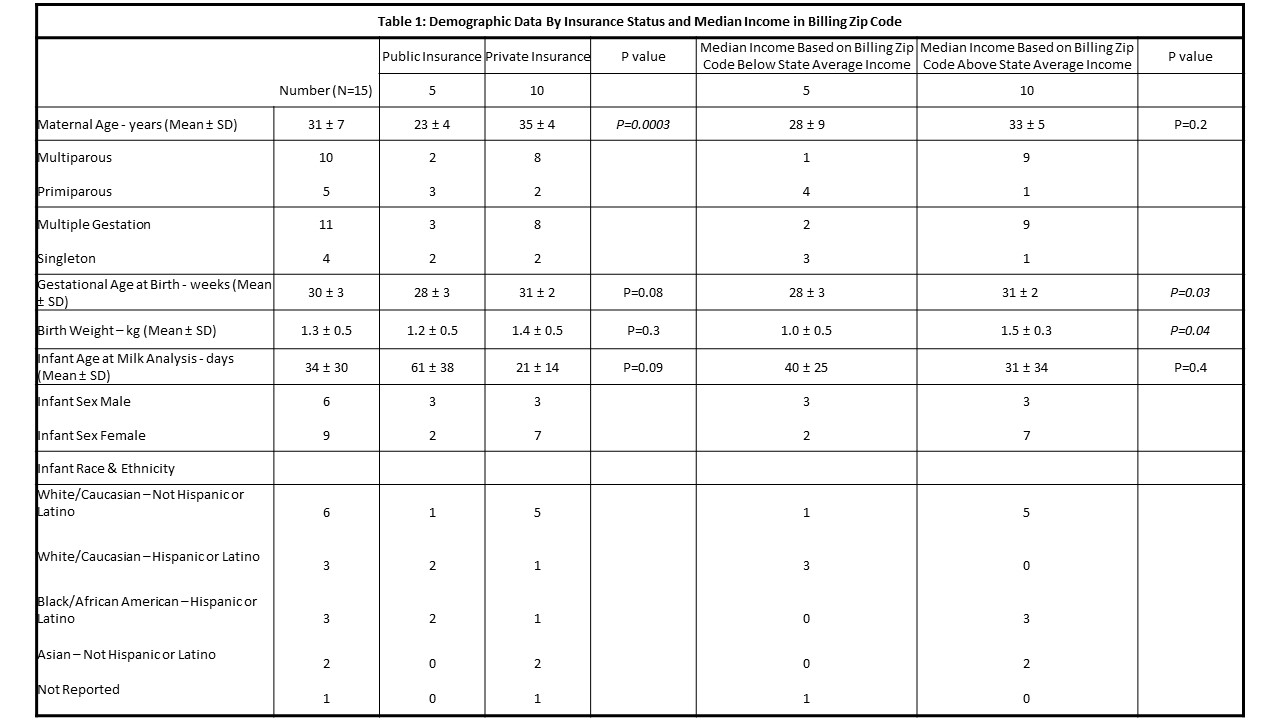
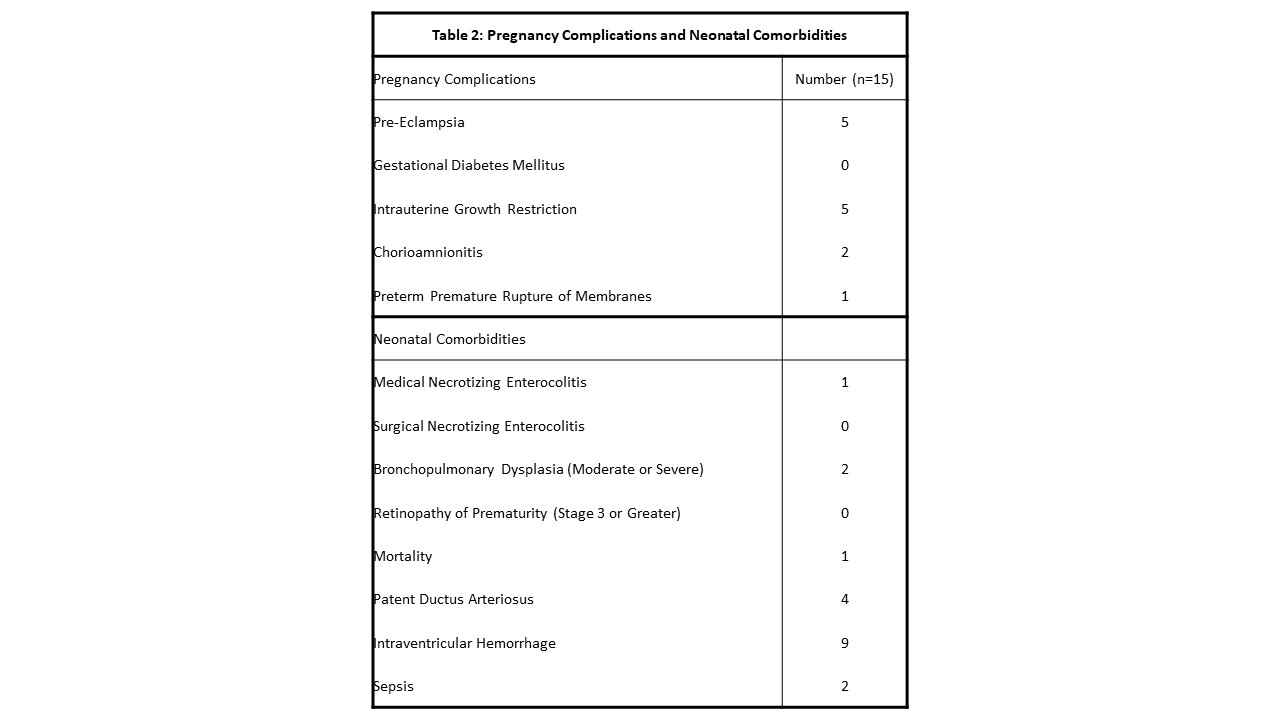
Results: Maternal milk for 36 infants was analyzed. 15 infants met inclusion criteria. Table 1 describes maternal and infant demographic data by insurance status and median income in the billing zip code. Table 2 includes pregnancy complications and neonatal comorbidities. MBM energy and macronutrient content was not correlated with median income in the billing zip code. MBM from mothers with private insurance had higher energy content than those with public insurance (84 ± 9 vs. 73 ± 6 kcal/100 ml, P=0.02), higher protein content (1.3 ± 0.2 vs. 1.0 ± 0.3 g/100 ml, P=0.03), and higher fat content (4.8 ± 0.9 vs. 3.8 ± 0.7 g/100 ml, P=0.04). Carbohydrate content was similar. Daily weight gain during admission was similar between groups.
Conclusion(s): MBM composition varied by public versus private insurance status, although infant growth was similar between groups and not correlated with maternal billing zip code median income. This highlights SDH and systemic inequities may impact human milk composition, indicating an area for further investigation.