Mental Health
Session: Mental Health 2
564 - Context and Management of Violent Patient Behaviors in a US Children’s Hospital
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 564
Publication Number: 564.1873
Publication Number: 564.1873
- AD
Adrienne DePorre, MD (she/her/hers)
Hospitalist
Children's Mercy Hospitals and Clinics
Childrens Mercy Kansas City
Prairie Village, Kansas, United States
Presenting Author(s)
Background: Behavioral dysregulation is common among hospitalized children and can escalate to physical violence towards others. Behavioral events in the hospital setting are a growing concern, contributing to reduced staff safety, poor patient outcomes, and increased hospital costs. Demographic and clinical factors associated with behavioral events are poorly described, especially within the inpatient pediatric setting. A better understanding of these contexts is critical to inform efforts to mitigate violent behaviors.
Objective: To describe physically violent patient behaviors and explore characteristics of hospitalizations associated with physically violent behaviors in the pediatric hospital setting.
Design/Methods: Utilizing both our electronic health record and the Pediatric Health Information System (PHIS) database, we conducted a retrospective single-center (no associated psychiatric unit) study of disruptive patient behaviors with physical violence from 2017–2022. We described and categorized the setting, antecedents, and staff management of violent behavior. To minimize bias in categorizations, two authors independently reviewed events. We also described characteristics of hospitalizations associated with physically violent behaviors.
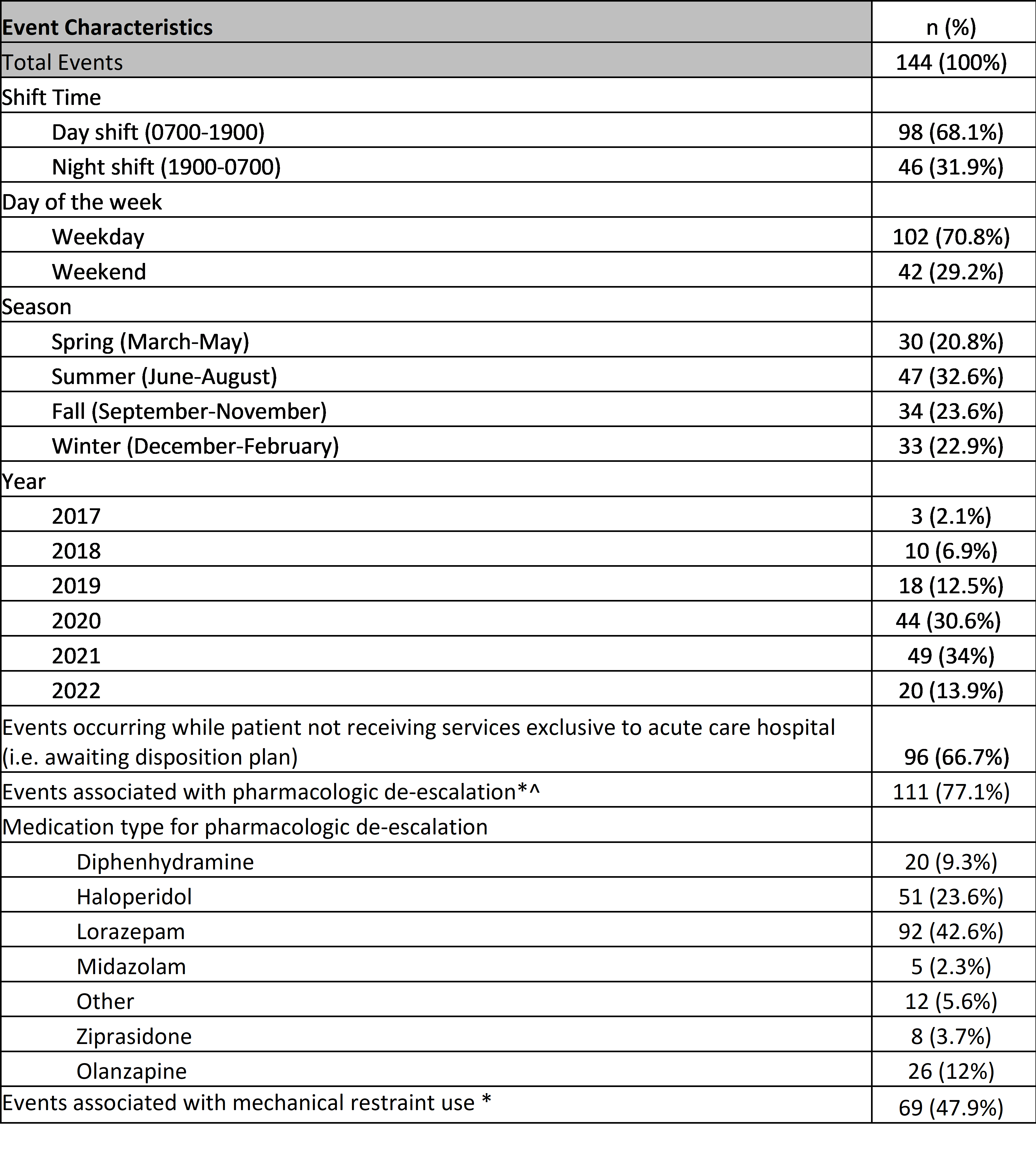
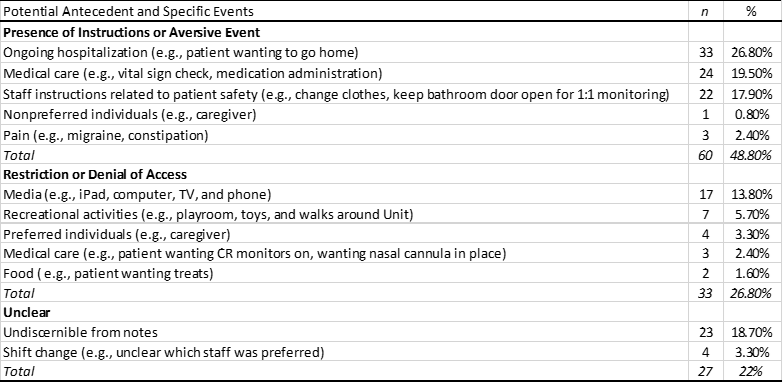
Results: We identified 144 behavioral events with physical violence associated with 85 hospitalizations (78 patients). The majority (68.1%) of events occurred during daytime hours, and there was no difference in event frequency by day of week. Most (66.7%) events occurred while a patient was awaiting safe placement/disposition and not needing hospital-level medical services. Pharmacologic de-escalation and mechanical restraints were associated with 77.1 % and 47.9 % events, respectively (Table 1). Violent behavior was most frequently preceded by aversive experiences such as ongoing hospitalization itself (26.8%), medical care (19.5%), and staff instruction (17.9%) (Table 2). The median number of events per hospitalization was 1 [IQR 1,2]; at the extreme, 5 hospitalizations accounted for 30% of events in the sample. Most (64.7%) hospitalizations with violent events had a primary mental health admission reason, and the plurality (44.7%) resulted in transfer to a different facility (Table 3).
Conclusion(s): Improved understanding of pediatric patient related physical violent events can aid in mitigating violent events, staff training/education and resource allocation. The social contexts (e.g., avoidance of aversive events) in which behavioral events occur can directly inform development of tailored behavioral support plans, and in turn improve patient and staff wellbeing.
.png)
