Neonatology
Session: Neonatal General 4: Nutrition, Feeding, and Growth
93 - The impact of exclusive human milk diet on short-term growth among very preterm infants
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 93
Publication Number: 93.296
Publication Number: 93.296
- FC
Fu-Sheng Chou, MD PhD (he/him/his)
Neonatologist
Kaiser Permanente Riverside Medical Center
Riverside, California, United States
Presenting Author(s)
Background: Exclusive Human Milk Diet (EHMD) involves fortifying human milk base with a human milk-based fortifier. EHMD has been proven to be cost effective in reducing the occurrence of necrotizing enterocolitis (NEC) and other complications of preterm birth. However, the negative impact of EHMD on postnatal growth has been suggested in the literature. For level 2 and 3 community neonatal intensive care units (NICUs) where NEC rates are low, the benefits of EHMD may need to be weighed against its impact on postnatal growth.
Objective: This study aims to investigate postnatal growth during EHMD administration.
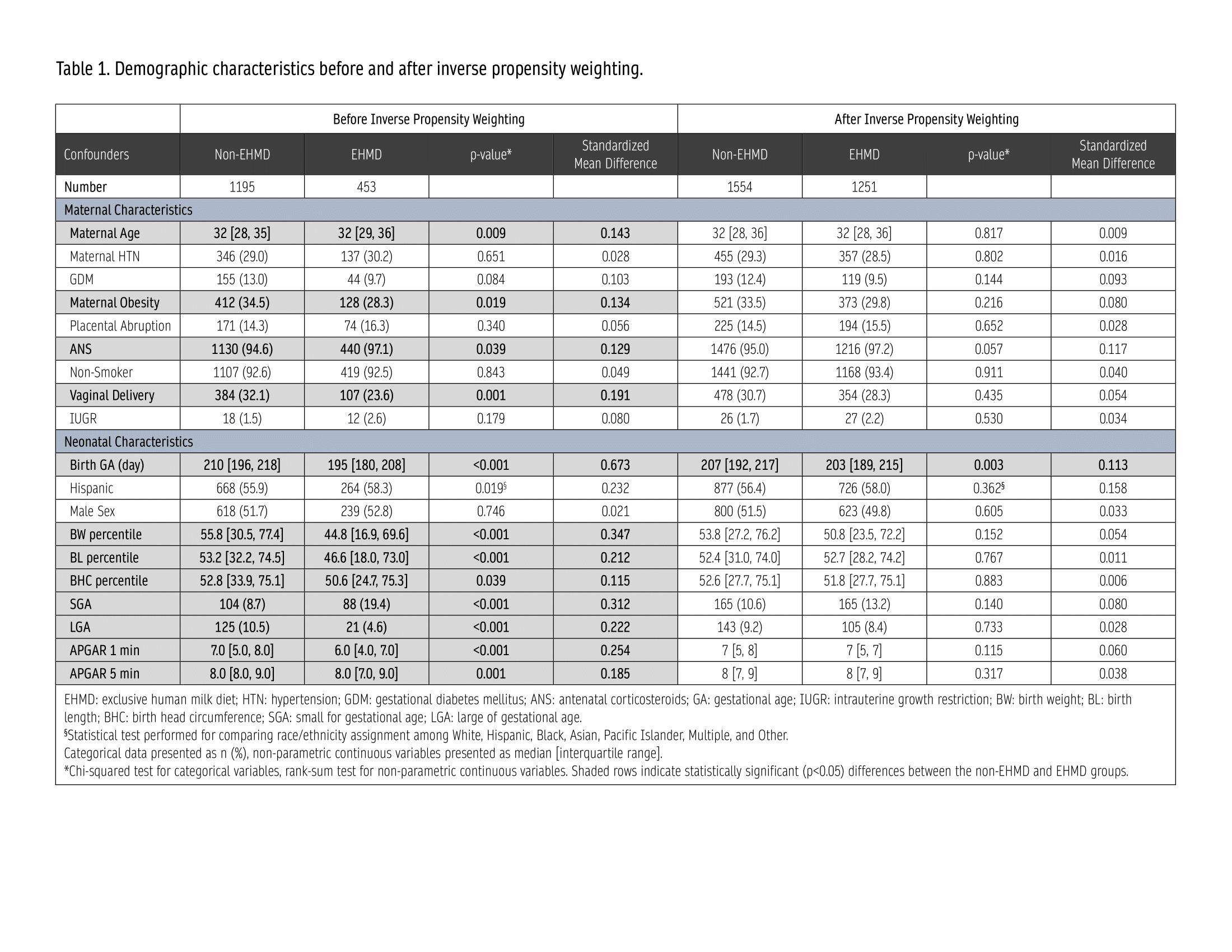
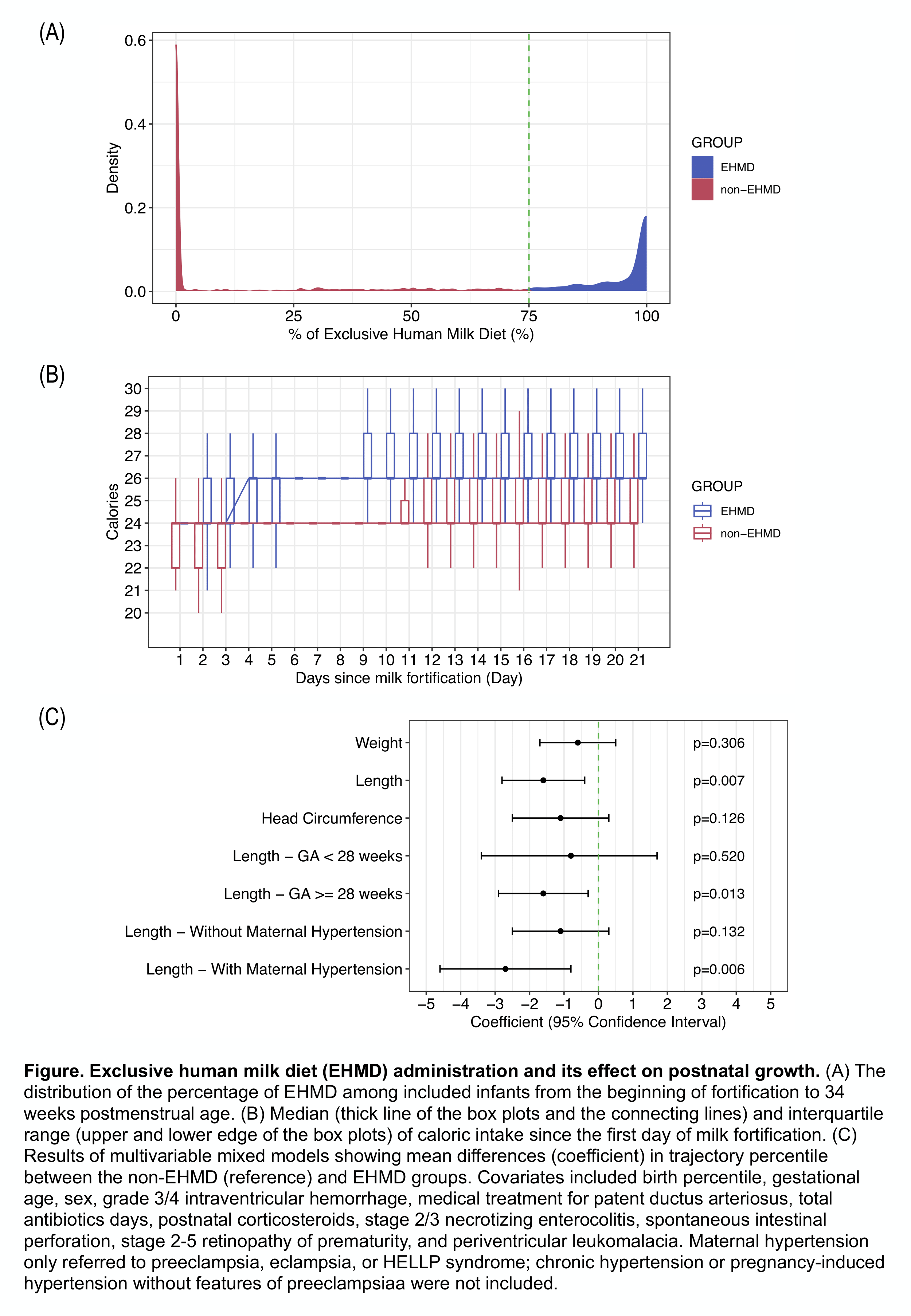
Design/Methods: A hypothetical multi-center target trial was emulated for infants born < 32 0/7 weeks’ gestation at Southern California Kaiser Permanente (SCAL-KP) from 2018 to 2022. Infants with major congenital anomalies, lost to follow-up at SCAL-KP before 6 months of corrected age (including death), and infants without enteral feeding data by 4 weeks of age, without caloric or growth data were excluded. Inverse propensity weighting (IPW) was used to control for confounders (Table 1) before EHMD prescription. The percentage of days receiving EHMD (%EHMD, determined by using physician orders) between the first day of milk fortification until 34 weeks postmenstrual age (PMA) was calculated (Figure 1A). Infants with ≥ 75% EHMD feeds were assigned to the EHMD group. Primary outcomes include trajectory percentiles (TP) using the Postnatal Growth Charts for Preterm Infants (PMID: 37726287). Multivariable mixed regression models were developed to assess the impact of EHMD on TP. Post-hoc subgroup analyses were performed.
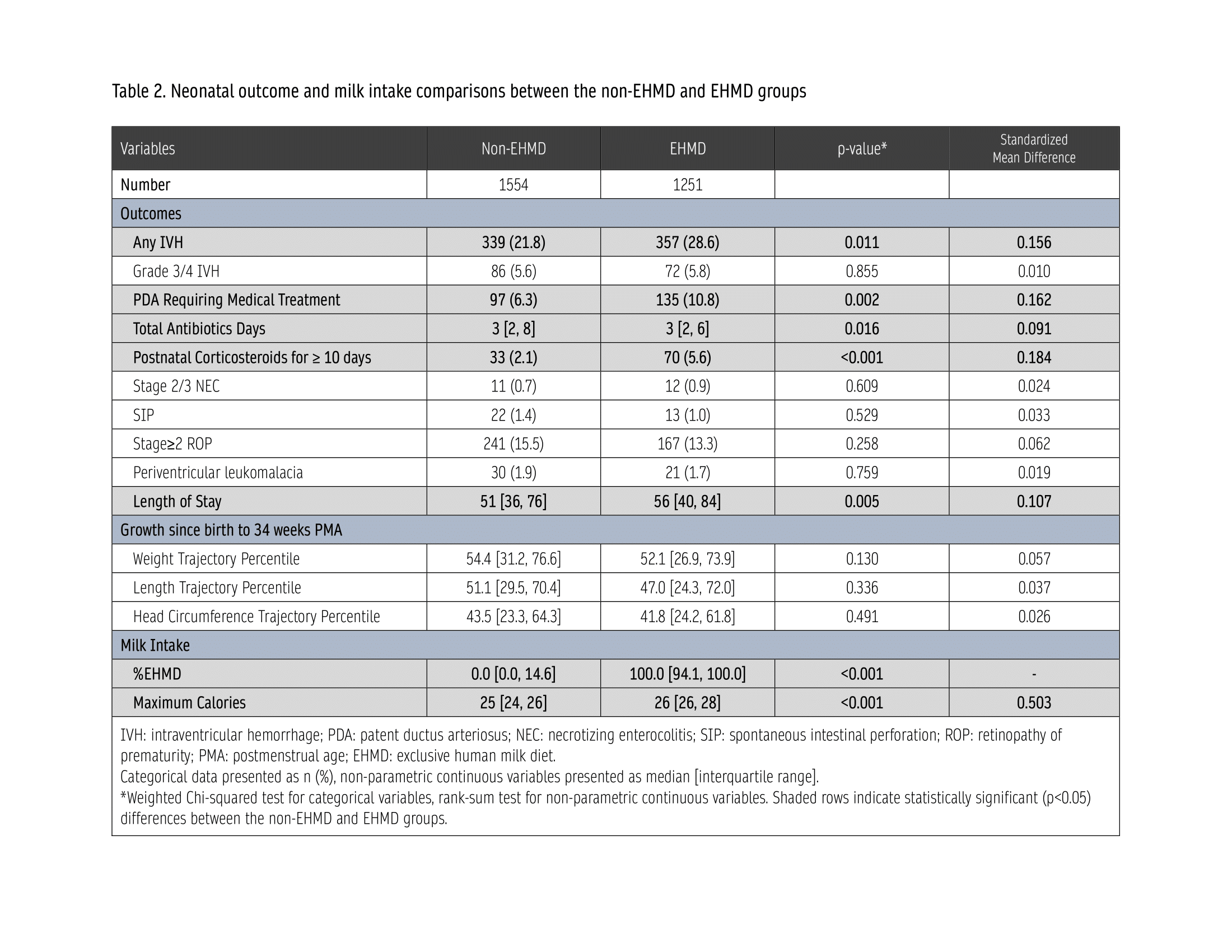
Results: 1648 infants were identified. After IPW, the pseudopopulation consisted of 2805 infants (1554 in non-EHMD and 1251 in EHMD groups) (Table 1). The median %EHMD was 0% (IQR: 0-14.6%) in the non-EHMD group and 100% (IQR: 94.1-100%) in the EHMD group. Figure 1B shows median caloric intake by day of fortification in both groups. Infants in the EHMD group had higher acuity of illness (Table 2). The multivariable models showed no differences in weight or head circumference TP between the two groups, but a reduction in length TP by 1.6% (95% CI:1.4-2.8%) in the EHMD group (Figure 1C). In subgroup analyses, reduced length TP was only observed in infants with birth GA ≥ 28 weeks (by 1.6% [0.3-2.9%]) or with exposure to maternal hypertension (by 2.7% [0.8-4.6%]) (Figure 1C).
Conclusion(s): EHMD is independently associated with reduced length growth, especially in infants with higher GA and exposure to maternal hypertension. A risk-stratified feeding protocol may be beneficial.