Neonatology
Session: Neonatal Fetal Nutrition & Metabolism 2: Fetal/Neonatal Metabolic Dyscrasias
135 - Agreement between point of care and serum glucose measurements in a newborn population
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 135
Publication Number: 135.626
Publication Number: 135.626
- DD
Daniela Dinu, MD
Associate Professor
Baylor College of Medicine
Houston, Texas, United States
Presenting Author(s)
Background: Neonatal glucose derangements are common metabolic disorders with almost 10% of term newborns experiencing hypoglycemia and almost 50% of ELBW newborns having hyperglycemia and are associated with increased mortality and morbidity. While measurement of serum glucose remains the gold standard, point of care (POC) measurement is preferred due to decreased amount of blood necessary and rapidity of results. Devices approved for POC glucose measurements in intensive care settings must comply with a recommendation from International Organization for Standardization (ISO) of agreeing within ± 15% of the serum glucose value.
Objective: We aimed to evaluate the agreement between POC and serum glucose values in neonates.
Design/Methods: We retrospectively reviewed electronic medical records of the newborns admitted to Texas Children’s Hospital between January 2012 and December 2022. We included newborns with at least one pair of serum and POC glucose measurements obtained within ± 5 minutes of each other. The nearest serum and glucose values in time were paired and analyzed. Serum values were treated as the gold standard. Bias in POC glucose measurements was computed as POC value – serum value. The “agree_nest” function was used to compute the Bland-Altman method limits of agreement (LOA) for repeated measures. For repeated measures from the same patients, mixed effects linear models were used to test for associations of clinical variables with bias.
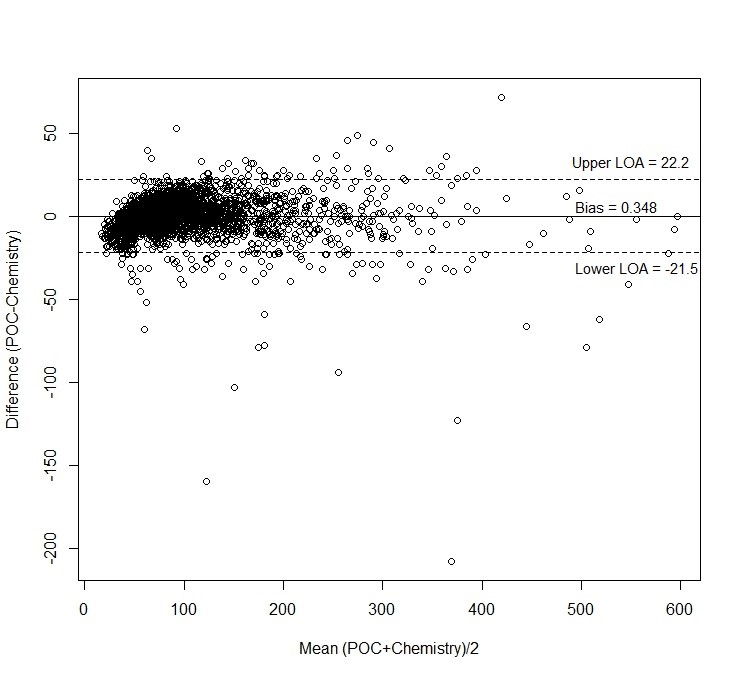
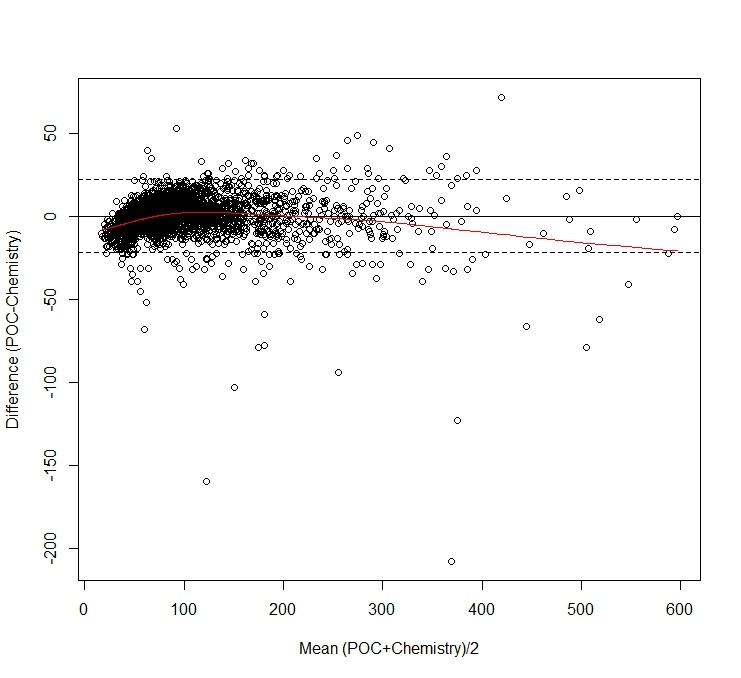
Results: We analyzed 3029 paired POC and serum glucose values from 1428 patients. The mean ± standard deviation of the bias was -0.038 ± 12.074 mg/dl (p=0.857). When accounting for repeated measures, the estimated mean bias was 0.348 mg/dl with LOA -21.503 to 22.199 mg/dL, beyond the acceptable ±15 mg/dl LOA (Figure 1, 2). The bias was not significantly associated with the mean of the serum and POC paired values (p = 0.838).
The model estimated mean bias was 2.49 mg/dl higher in preterm compared to term infants (p < 0.001). The bias was not significantly associated with the time difference between POC and serum (p=0.693), patient’s postmenstrual age (p=0.437) or chemistry being drawn from an arterial line (p=0.450).
Conclusion(s): The average POC bias is not statistically significant. However, the LOA for the POC are wider than the ± 15mg/dl LOA according to the ISO guidelines due to the large variation in the POC bias across samples. POC values tended to be lower than chemistry values at the lower and higher ends of the range. Thus, the results show that the POC measurements lack the precision to be used interchangeably with the gold standard serum glucose values.