Neonatology
Session: Neonatal/Infant Resuscitation 2
284 - “Where’s the cord gas?” Missed Opportunities for Neonatal Assessments When Standardized Guidelines for Collection are Not Established
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 284
Publication Number: 284.3128
Publication Number: 284.3128
.jpg)
Isabella T. Eiler, MD
Fellow
Children's Hospital of Wisconsin
Menomonee Falls, Wisconsin, United States
Presenting Author(s)
Background: Umbilical cord blood gas (UCBG) sampling for high-risk deliveries (HRD) serves as a biochemical marker for hypoxic ischemic encephalopathy (HIE). Lack of national guidelines has led to variable practice. We hypothesize that inconsistent UCBG sampling for HRD leads to missed opportunities for HIE assessment.
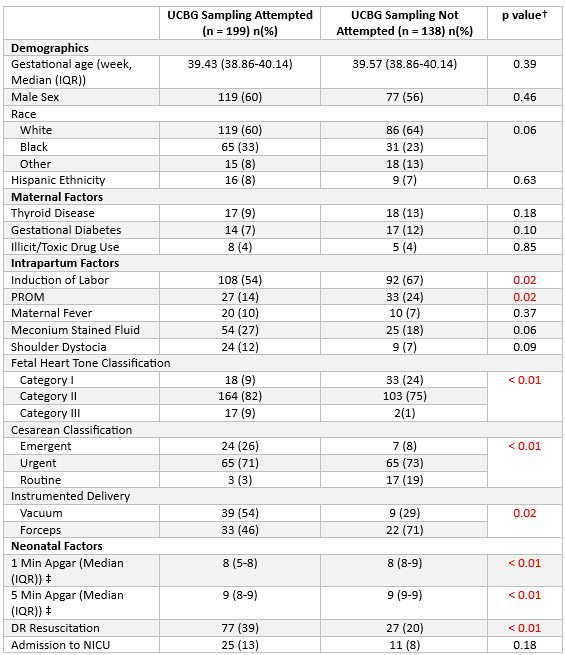
Objective: To determine the prevalence of UCBG sampling in HRD at a Level IV Perinatal Center. We compared maternal factors, delivery characteristics, and neonatal outcomes between infants who did and did not have UCBG sampling performed.
Design/Methods: A retrospective cohort study of all HRD for infants ≥ 36 weeks gestation was conducted from 1/2019-12/2019. HRD were defined by the presence of placental abruption, uterine rupture, cord prolapse, shoulder dystocia, delivery expedited with instrumentation or cesarean section for fetal intolerance, or a depressed infant defined by a 5-minute Apgar of ≤ 5. Our study cohort was divided into two groups: those who had UCBG sampling attempted vs. those who had not. Categorical variables were analyzed using the Chi-square or Fisher’s exact test, while continuous variables were evaluated with the Mann-Whitney test.
Results: We screened 3146 deliveries and found HRD to account for 12% of all deliveries. The prevalence of UCBG sampling in HRD was 59%. Of the infants with UCBG sampling attempted, 80% had arterial sample results (Figure 1). Mean gestational age was 39.3 weeks (range 36.1-42 weeks). The two groups did not differ in demographic or maternal health factors (Table 1). Intrapartum factors associated with lack of UCBG sampling were induction of labor, prolonged rupture of membranes, and forceps-assisted delivery. Infants with category III fetal heart tones, born via emergent cesarean, or required delivery room resuscitation were more likely to have UCBG drawn. Of infants admitted to the NICU, 31% had no UCBG. In the entire study cohort, one infant was diagnosed with severe HIE and had an UCBG drawn.
Conclusion(s): Delivery room management in HRD without standardized guidelines results in ~40% without UCBG sampling. Subsequently, many NICU admissions lacked biochemical criteria for HIE assessment. Next steps include assessing the impact on clinical care after implementation of multidisciplinary neonatal guidelines for UCBG response.
.png)