Adolescent Medicine
Session: Adolescent Medicine 1
145 - The association between resilience and mental health among adolescents and young adults during the pandemic
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 145
Publication Number: 145.436
Publication Number: 145.436

Lauren E. Wisk, PhD (she/her/hers)
Assistant Professor
David Geffen School of Medicine at UCLA
Los Angeles, California, United States
Presenting Author(s)
Background: Prior work shows that adolescents/young adults (AYA) were vulnerable to negative mental health during the COVID-19 pandemic.
Objective: We sought to take a positive youth development approach to understand the role of youth resilience in protecting against adverse mental health consequences of the pandemic.
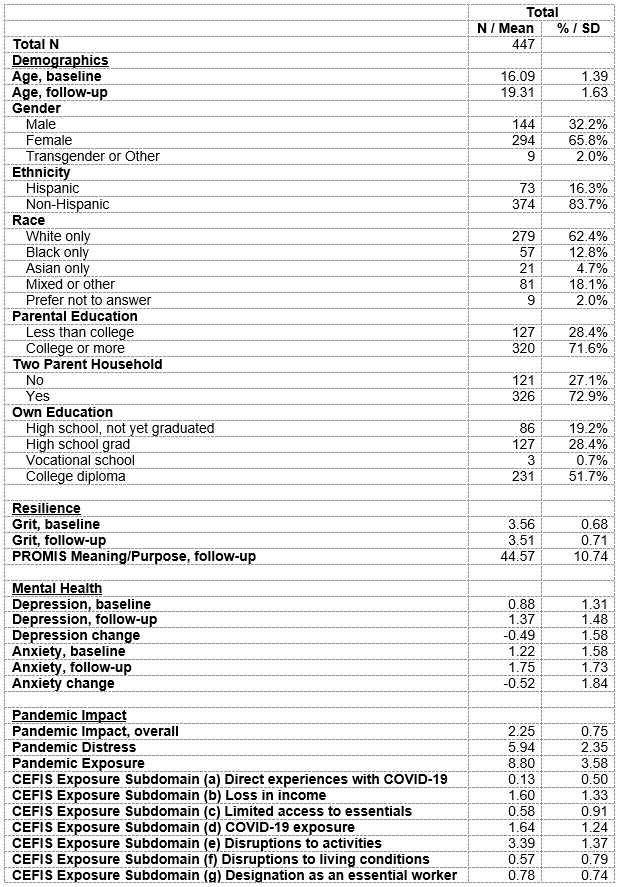
Design/Methods: Between 02/16-11/18, 975 AYA (ages 14-18 years) patients of a large academic medical center were recruited in an observational cohort study and RCT; 501 were subsequently enrolled in a follow-up study between 10/20-05/21. Information on resilience (GRIT; PROMIS meaning and purpose (MP)), pandemic impact (COVID-19 Exposure and Family Impact Scale, CEFIS), and mental health (PHQ-2 and GAD-2 for depression, anxiety respectively) were collected. Multivariable regression was used to assess how resilience impacted change in mental health, and to evaluate if pandemic impact moderated this association.
Results: Respondents were a mean age of 16.1±1.4 years at baseline; 65.8% female, 16.3% Hispanic, 62.4% white. Pre-pandemic youth reported minor depressive symptoms (PHQ-2 score of 0.88±1.31), with moderately higher anxiety (GAD-2 scores of 1.22±1.58). Peri-pandemic, youth had a significant increase in depressive symptoms (1.37±1.48, p<.001) and anxiety (1.75±1.73, p<.001). Youth reported moderate resilience (GRIT 3.51±0.71; MP 44.57±10.74). On average, youth reported moderate exposure to pandemic-related events (8.80±3.58, range:1-20), moderate perceived impact of the pandemic on social-emotional functioning (2.25±0.75, range:0-4), and moderate pandemic-related distress (5.94±2.35, range:1-10). Youth with higher reported GRIT scores at baseline had smaller adjusted increases in depression (β=-0.497, p<.001) and anxiety (β=-0.307,p=0.011) during the pandemic than those with lower scores. Higher MP scores were associated with similar protective effects against decrements in depression (β=-0.058,p <.001) and anxiety (β=-0.046,p <.001). Pandemic impact and distress were associated with worsening depression and anxiety (p <.001), while pandemic exposure was associated with increasing depression and anxiety (p < 0.05). There was not statistical evidence to support moderation between resilience and pandemic impact.
Conclusion(s): Consistent with other studies, we identified worsening mental health during the pandemic. Youth with greater resilience experienced protection against mental health declines peri-pandemic. While we did not find evidence of moderation, the magnitude of the independent effect of resilience is such that it can meaningfully buffer the impacts of the pandemic to protect health.