Neonatology
Session: Neonatal-Perinatal Health Care Delivery: Practices and Procedures 1
446 - Decreasing Unplanned Extubation Rate Using Innovative 3D Printing Technology
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 446
Publication Number: 446.2914
Publication Number: 446.2914
- AZ
Alla Zaytseva, MD (she/her/hers)
Neonatal-Perinatal Medicine Attending
Cohen Children's Medical Center
new hyde park, New York, United States
Presenting Author(s)
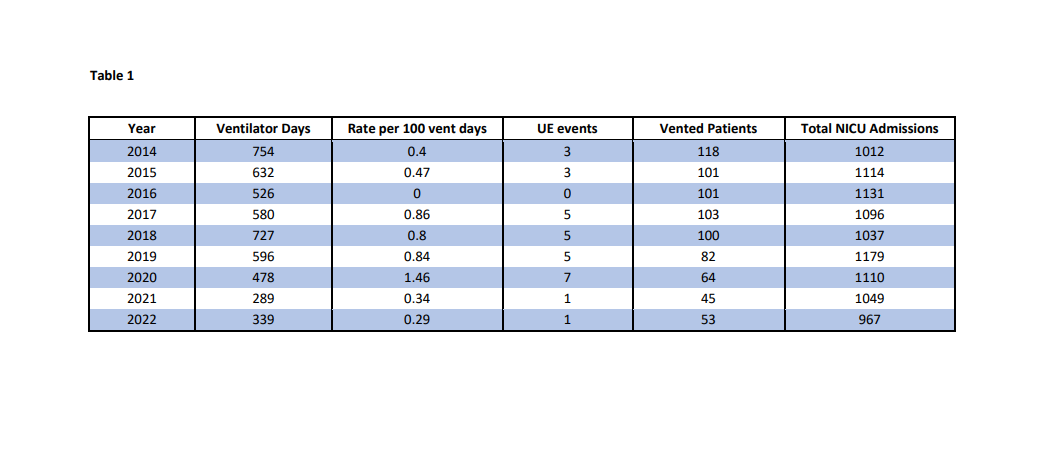
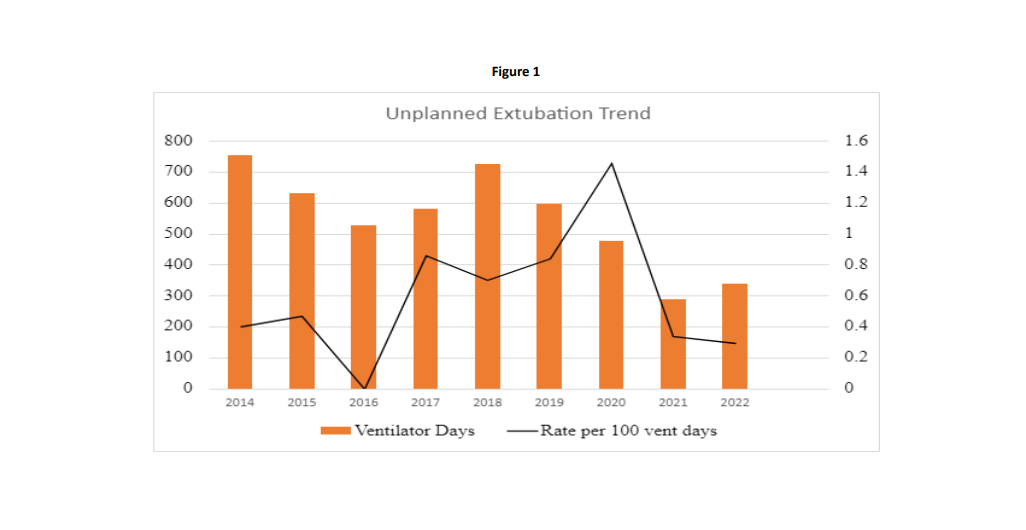
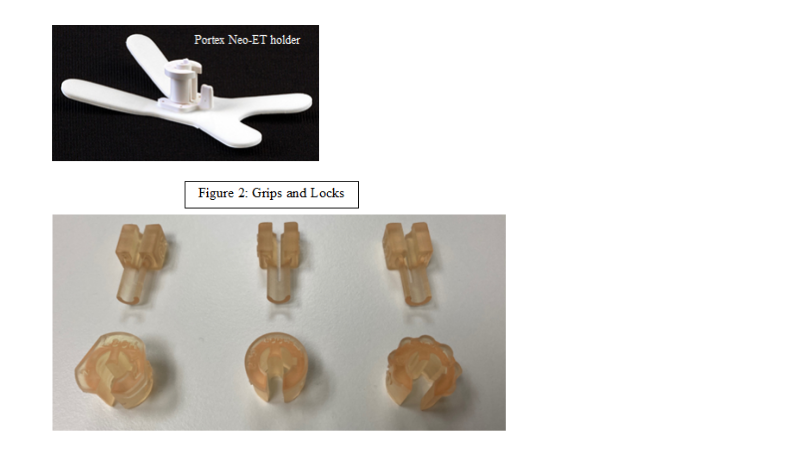
Background: Unplanned extubation (UE) in NICU continues to be a dangerous yet relatively frequent event. Variable endotracheal tube (ETT) stabilizing devices are commercially available with strong user preference. In our level III NICU, dedicated respiratory therapists (RTs) manage ETT securement and adjustments. We successfully used Protex neo-ETT holder kits by Smith Medical for over 10 years, with UE rate remaining < 0.5/year. In 2015 the ETT holder for < 3.5 ETT were discontinued and by 2017 our supplies where exhausted. We transitioned to 3M tape, a significantly different securement technique. During this time the rate of UE continued to increase to a peak of 1.4 in 2020, despite the introduction of validated UE bundle used at our system level NICUs and the creation of an interdisciplinary task group. Focus on non-invasive respiratory management such as bubble CPAP and Least Invasive Surfactant Administration (LISA) in 2019 and 2020 decreased the number of intubated patients, in turn limiting RTs ability to acquire expertise and comfort with 3M tape securement devise. In 2020 we approached Northwell 3D Designs and Innovation Department to create a prototype lock for < 3.5 size ETT to be used with Protex neo-ETT 3.5 base.
Objective: To reduce and maintain UE number to < 0.5 per 100 ventilator days by using innovative 3D printing lock to fit established and familiar ETT securement device.
Design/Methods: 3D Department reverse engineered 3.5 ETT base and created 3D printed via stereolithography using biocompatible photopolymeric resin twist-locking holder locks for 2.0, 2.5 and 3.0 ETT that fit 3.5 Protex base. The locks were tested to maintain inner ETT diameter, provide fixed hold in lock position, ease of identification based on size and ease of single provider use. To prevent ETT migration when the lock is in an open position for ETT adjustment, a removable grip was created. After successful patient trials, the unit transitioned to the 3-D print lock in early 2021.
Results: Since implementation of 3D print lock, UE rate decreased to 0.34 in 2021 and continued to decrease to 0.29 in 2022, surpassing our goal despite significant decrease in both number of intubated patients and ventilator days.
Conclusion(s): The use of innovative technologies, such as 3D printing of ETT securement devices can mimic familiarity with well-known and successful but since then discontinued devices, improving patient safety and decreasing UE rate. We speculate that our improved UE rate compared to the pre 2017 baseline is due to composite effect of UE bundles and interdisciplinary task group work on use of 3D printed ETT lock.