Technology
Session: Technology 2
182 - Artificial Intelligence for Precision Medicine in Preterm Infants
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 182
Publication Number: 182.2077
Publication Number: 182.2077

Rema A. Zebda, DO
Neonatology Fellow
Texas Children's Hospital
Houston, Texas, United States
Presenting Author(s)
Background: Prematurity continues to be an unsolved problem in the US, leading to long-lasting health problems in premature infants and significant financial and psychosocial burden on families. Preterm infants born < 1500g (very low birth weight, VLBW) experience increased mortality (10-15%) and only 70% survive without major morbidity. Our aim is to leverage machine learning to develop predictive models for mortality and 5 major morbidities in preterm infants – including bronchopulmonary dysplasia (BPD), retinopathy of prematurity (ROP), necrotizing enterocolitis (NEC) sepsis/meningitis, and intraventricular hemorrhage (IVH).
Objective: The objective of this study is to develop robust machine learning models, integrating a multitude of clinical variables in the first 2 weeks of life that will reliably predict survival and morbidity in VLBW infants. We believe that accurate predictive models will encourage timely interventions in individual patients and will foster targeted precision medicine.
Design/Methods: Methods: We used a retrospective cohort from the Vermont Oxford Database (VON) from Texas Children’s Hospital (n=3508 VLBW infants) to validate the model and test on Texas Children’s Hospital Neonatal Consortium data (n=455 VLBW infants). We integrated 48 clinically significant variables into these predictive models. Several standard multivariate algorithms were compared, including Random Forest (RF), XGBoost, Logistic Regression, Support Vector Classification. All models were evaluated by implementing a 10-fold CV strategy on the first dataset and retrained to test on the second dataset for final performance.
Results:
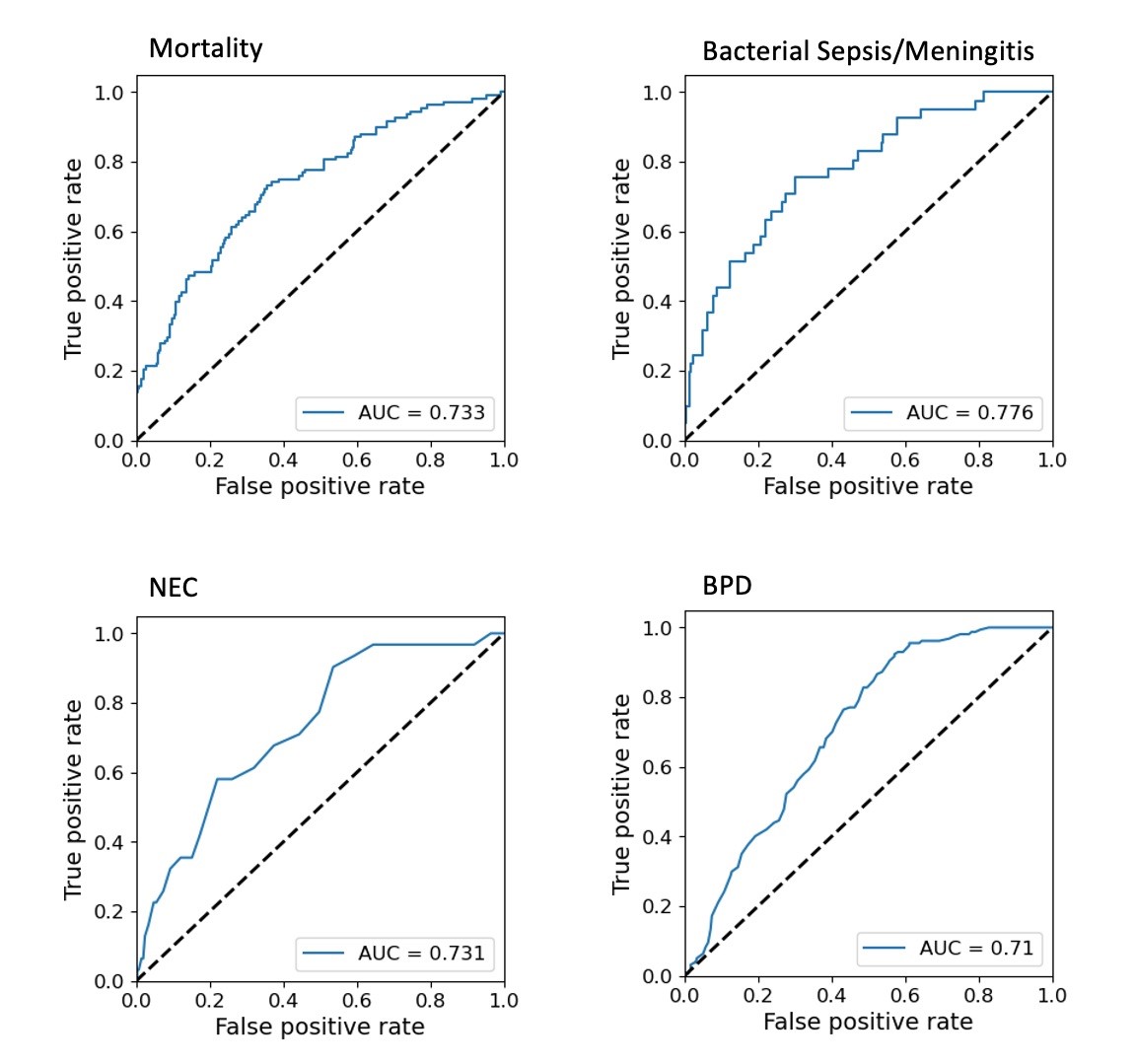
Results: For all 6 morbidity and mortality outcomes (BPD, ROP, NEC, sepsis/meningitis, and IVH) we built models generating significantly different risk scores among case and control patients. Tree-based ensemble models, RF and XGBoost, have the best performance among five of them. Area Under the Receiver Operating Characteristic (AUROC) of sepsis and/or meningitis (0.73), NEC (0.73), BPD (0.71) and mortality (0.74) exceed 0.7, suggesting the capability of early outcome detection.
Conclusion(s):
Conclusions: Harnessing the power of AI, our goal was to use the formulated clinical predictive models, where outcomes can be predicted in advance and by proactive management, will change health trajectory towards better outcomes. We believe that our research will facilitate a paradigm shift from reactive medicine to proactive precision medicine within Neonatology.