Technology
Session: Technology 2
185 - Assessment of heterogeneity in prehospital team communication during teleconsultations with pediatric emergency physicians in simulated critical pediatric transports.
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 185
Publication Number: 185.2080
Publication Number: 185.2080

Ryan Brewster, MD (he/him/his)
Resident Physician
Boston Children's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Expert teleconsultation as a prehospital intervention may improve pediatric outcomes. Gaps in physician training for emergency medical services (EMS) medical oversight may lead to variability in how physicians and EMS personnel communicate during teleconsultation which could moderate intervention effects.
Objective: To prepare for a future trial, we measured adherence to communication best practices in paramedic-physician teams (prehospital teams) using teleconsultation in simulated pediatric transports.
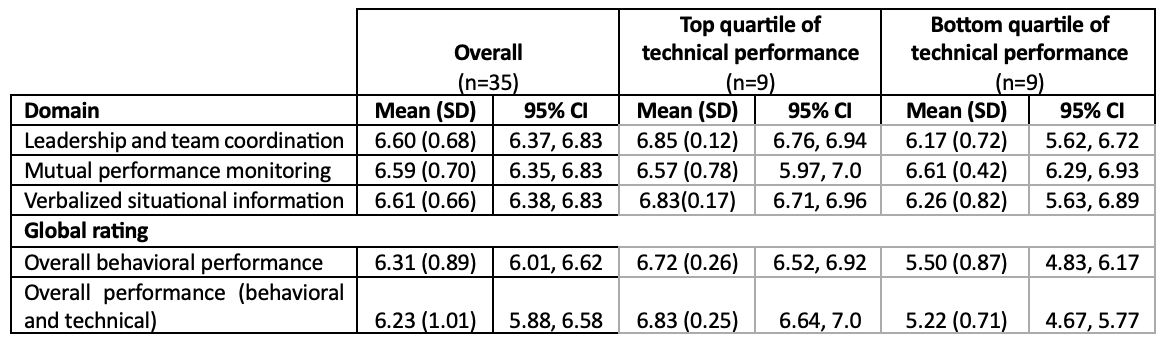
Design/Methods: This was a secondary analysis of video recordings of paramedic dyads in ambulances using teleconsultation with a remote pediatric emergency physician in a simulation model of 3 pediatric transport scenarios (cardiac arrest, asthma, seizure). Two raters, blinded to technical performance, used the University of Auckland Behavior Rating Scale to score the frequency of observed teamwork behaviors in 3 communication domains - leadership and team coordination, mutual performance monitoring, and verbalized situational information. Raters scored 7-point Likert scales for 23 behavior items (1=Never/rarely, 7=Consistently) and global ratings of behavioral and overall performance (1=Poor, 7=Excellent). We measured technical performance on a simulation checklist for each scenario. We defined adherence to communication best practices (primary outcome) as a mean teamwork score ≥6 averaged across raters for all behavior items. Secondary outcomes were mean domain scores, and behavioral and overall performance ratings. We used descriptive statistics and grouped transports into top and bottom quartiles of technical performance to report the proportion of teams meeting adherence criteria per group. We explored if teamwork could predict technical performance variation controlling for team and scenario using linear models without correlated observations.
Results: Twelve prehospital teams completed 3 simulated transport scenarios each, of which 35 (97%) video-recordings were available for analysis. The mean teamwork score was 6.60 (95% CI 6.39, 6.81). Table 1 summarizes secondary outcomes. All teams in transports in the top quartile of technical performance met adherence criteria as compared to 78% of teams in transports in the bottom quartile. Teamwork did not predict technical performance after controlling for team and scenario (p=0.86).
Conclusion(s): Prehospital teams used communication best practices frequently during teleconsultation in simulated pediatric transports. While teams with the highest technical performance exhibited these behaviors most often, teamwork did not predict technical performance.