Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 3
12 - Timely Discharges: A Resident Led Quality Improvement Project on Improving Timeliness of Discharge Order Placement
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 12
Publication Number: 12.2941
Publication Number: 12.2941

Ancil J. Abney, MD (he/him/his)
Pediatric Hospitalist/Inpatient Rotation Director
Arnold Palmer Hospital for Children
Winter Park, Florida, United States
Presenting Author(s)
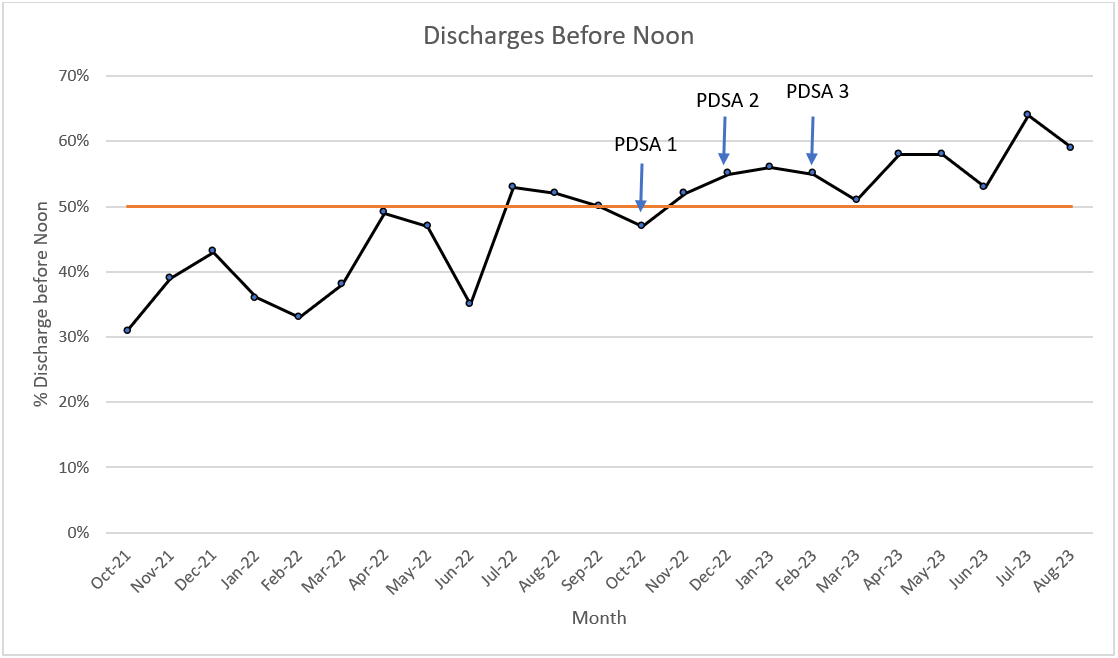
Background: Unnecessary delays in discharge timing create an inability to maintain patient flow out of the hospital and limits the ability to provide effective and timely care to patients that need it. This creates artificial bottlenecks and prevents the full utilization of other hospital departments contributing to patient safety issues in the emergency department, work compression for staff, and prolongs length of stay. Our hospital medicine group had an average rate of 35% of discharge orders being placed before 12:00.
Objective: A resident-led QI team will increase the average percentage of discharge orders placed by 12:00 from 35% to 50% within 6 months.
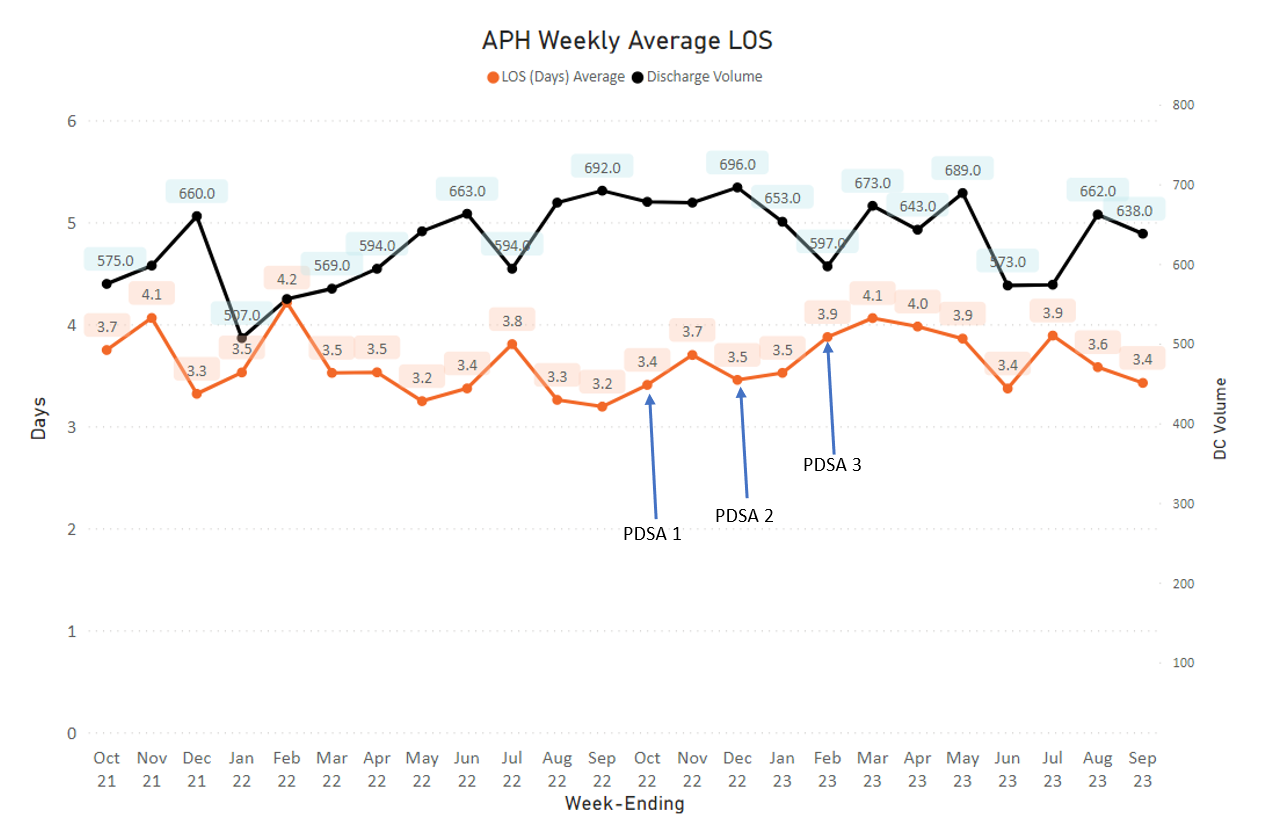
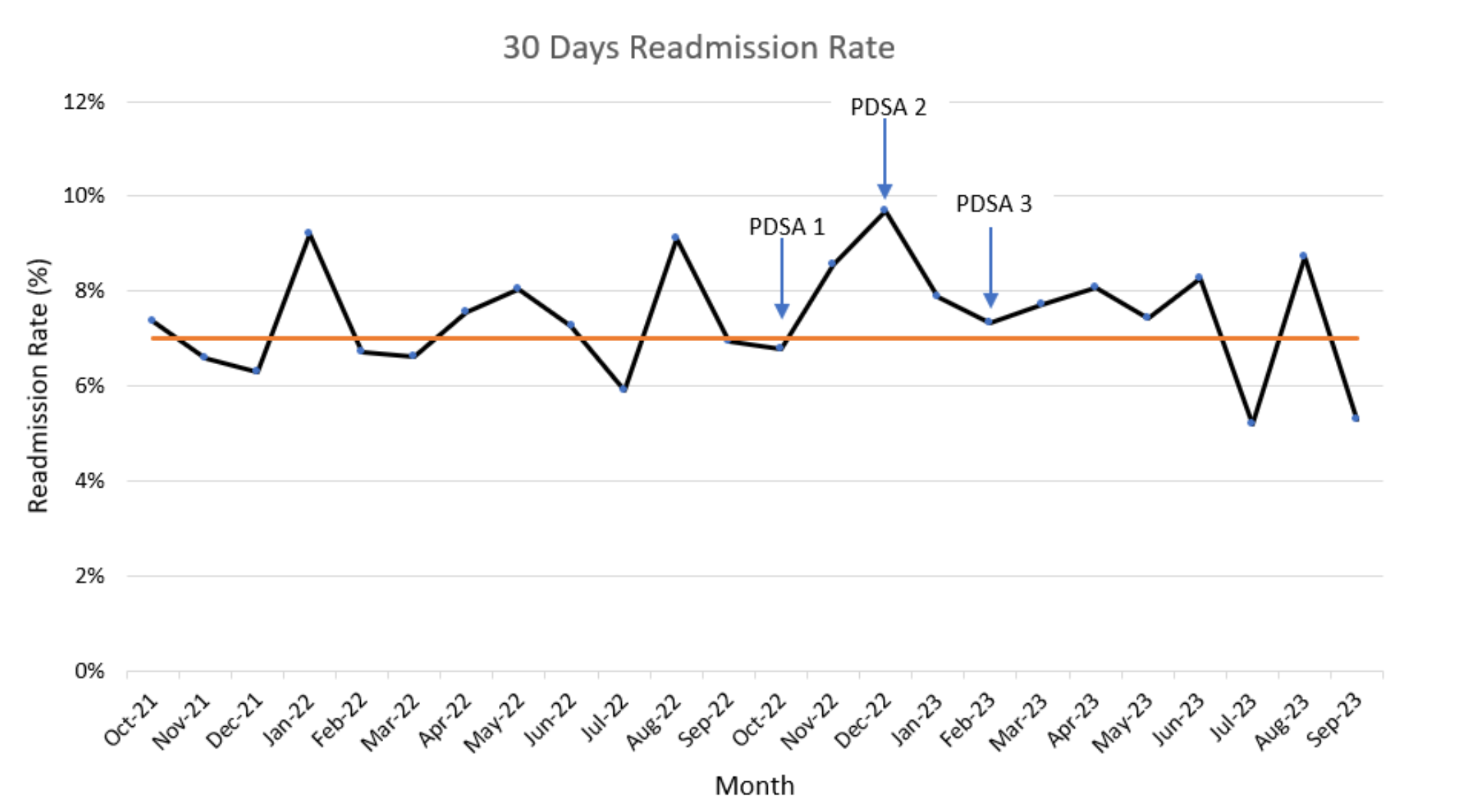
Design/Methods: This was a QI project where we evaluated discharge order placement times and implemented multiple changes in 3 consecutive PDSA cycles. A multidisciplinary team consisting of attending physicians, resident physicians, a QI specialist, and nursing leadership. PDSA cycles included education of attendings to round early on discharges (cycle 1), education and weekly reminders for senior residents to prioritize discharges on rounds (cycle 2), and placing discharge orders prior to starting rounds via text communication between attending and senior resident. The primary outcome measure of our project was discharge order placement rates before 12PM. Secondary outcome measures included time from discharge order to time of discharge. Balancing measures included average length of stay and readmission rates to ensure that we did not unnecessarily impact patient care during this process.
Results: The average discharges placed before noon improved with each PDSA cycle resulting in an average of 58% of discharge orders being placed before noon (figure 1). Readmission rates (figure 2) and length of stay (figure 3) remained unchanged during the project's duration with only expected seasonal variation.
Conclusion(s): Identifying non-complex discharges and allowing the attending and senior resident to prioritize these discharges prior to teaching rounds improves the ability of teams to complete discharge tasks earlier without increasing length of stay or increasing readmission rates. Future interventions to address length of stay and throughput include brief afternoon discharge readiness rounds.