Neonatology
Session: Neo-Perinatal Health Care Delivery 1: Epidemiology/Health Services Research
312 - Black Women with High-Risk Pregnancies: Results from a Randomized Controlled Trial of the Preemie Prep for Parents (P3) Program
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 312
Publication Number: 312.1385
Publication Number: 312.1385
- SM
Siobhan M. McDonnell, MS (she/her/hers)
Clinical Research Assistant
Medical College of Wisconsin
Willmar, Minnesota, United States
Presenting Author(s)
Background: Every day more than 200 Black women in the US deliver preterm. Despite greater prevalence of medical conditions that lead to preterm birth, Black women are less likely to receive prenatal education on measures recommended by the American College of Obstetricians and Gynecologists (ACOG) to reduce preterm births. We have developed the smartphone Preemie Prep for Parents (P3) program to address this gap in prenatal education.
Objective: Examine the effect of the P3 program on knowledge of preterm birth and preparation to make healthcare decisions among Black pregnant women.
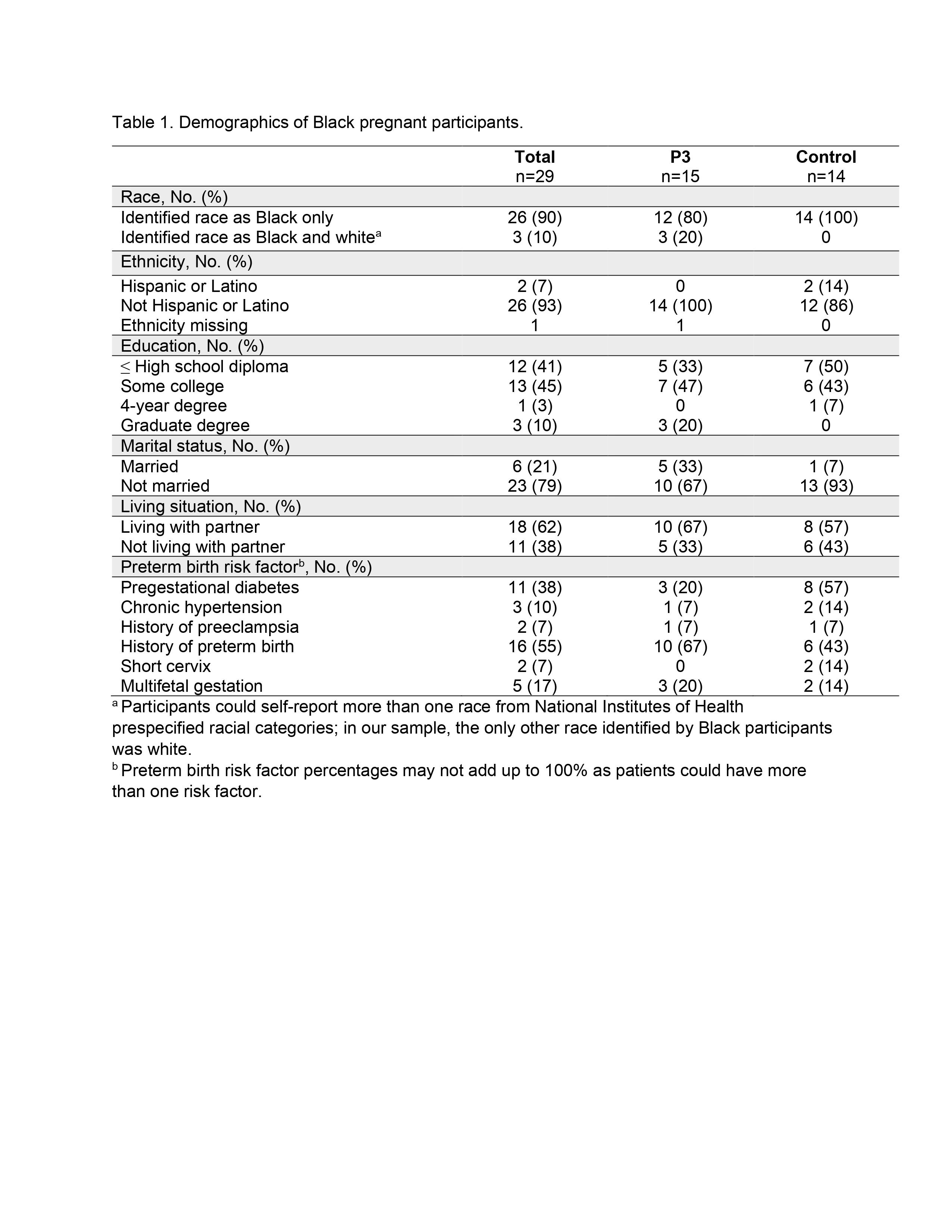
Design/Methods: This is an ancillary analysis of a randomized controlled trial (NCT04093492) of pregnant women with medical conditions that predispose to preterm birth. The P3 group received periodic text messages, starting as early as 18 weeks gestational age (GA) and until preterm birth or 34 weeks GA. Each P3 text message had a link to 1 of 51 short, animated videos. The control group received links to ACOG patient education webpages. At 25, 30, and 34 weeks GA, participants completed a knowledge questionnaire, Preparation for Decision Making Scale, and PROMIS Anxiety scale. Upon study completion, subjective feedback was collected. This subgroup analysis examined responses from participants self-reporting as Black.
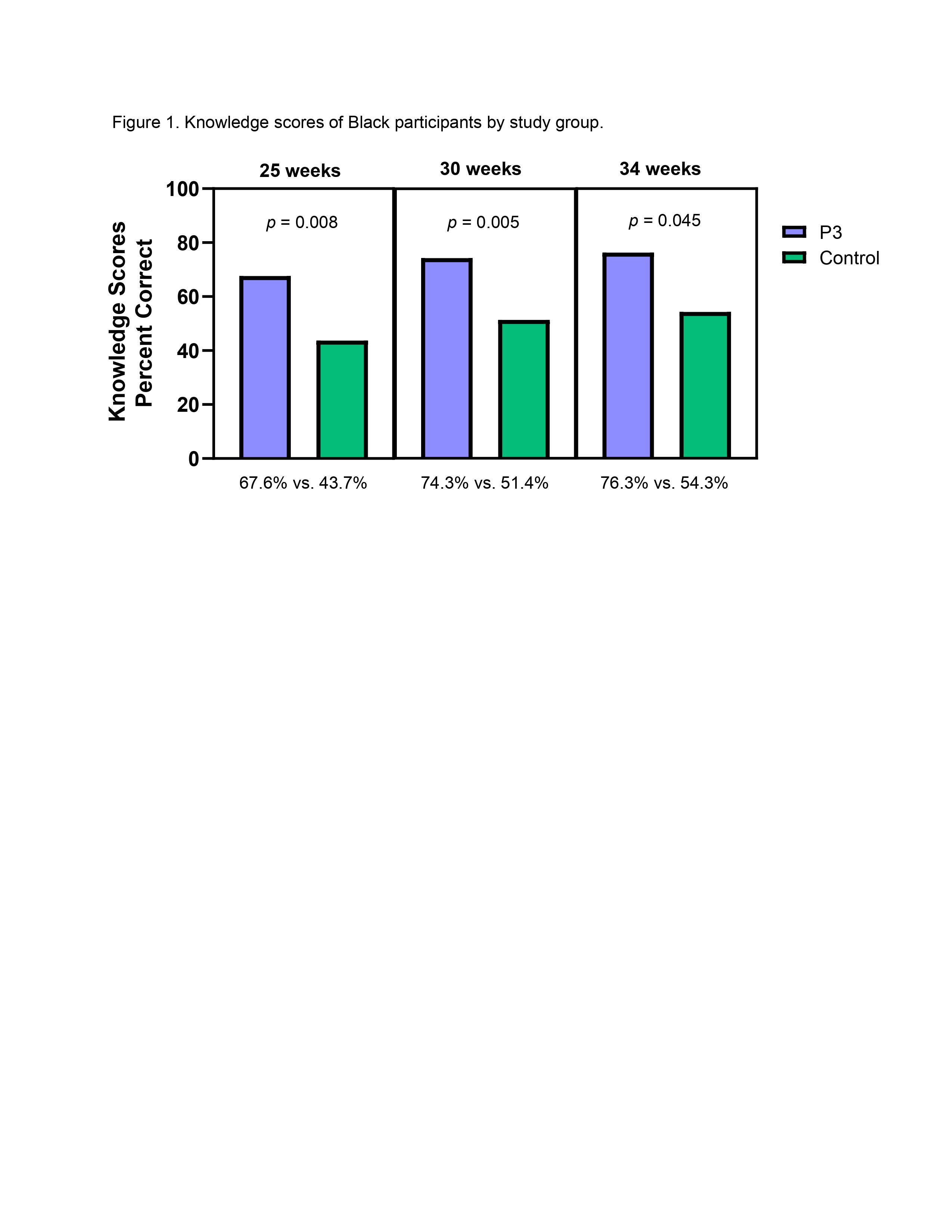
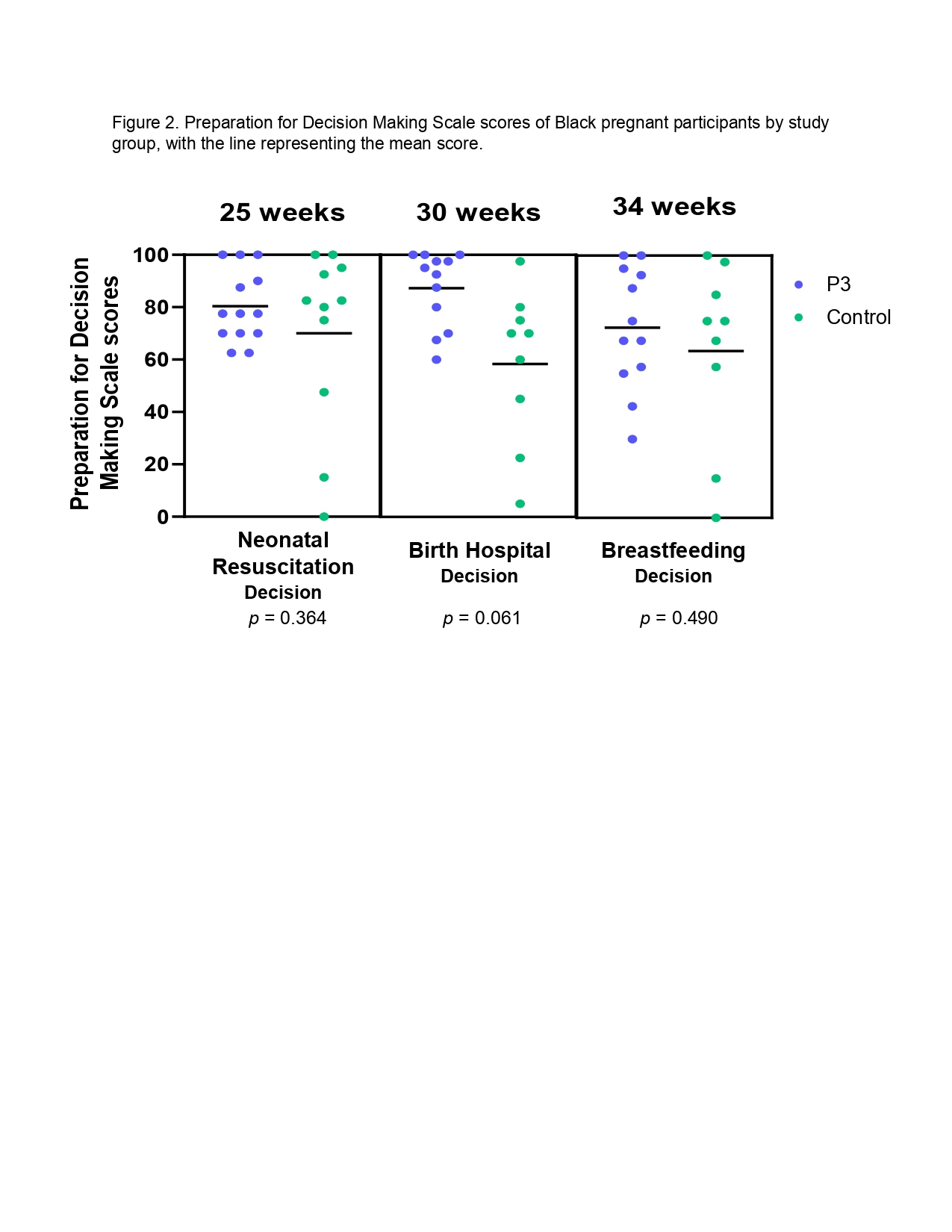
Results: A total of 121 Black women were contacted and 29 (24%) enrolled, Table 1. Maternal anxiety at 25, 30, and 34 weeks GA was not higher than baseline in either study group. At all 3 assessments, the P3 group (n=15) had more preterm birth knowledge than the control group (n=14), Figure 1. Preparation for Decision Making scores were not significantly higher in the P3 group (Figure 2), despite a trend. Compared to the control group, more women in the P3 group reported discussing preterm birth with their partner (100% vs. 56%) and sharing information with family and friends (58% vs. 44%). More participants in the P3 group reported that the study education provided more information on preterm birth than their physician (100% vs. 67%).
Conclusion(s): While this study is limited as a post-hoc analysis of a small sample, it shows that the P3 program offers a method to overcome barriers to prenatal education faced by Black women. Future work needs to address the low participation by Black women. However, even with current enrollment rates, this inexpensive and scalable program could potentially benefit thousands of Black families every year.