Neonatology
Session: Neonatal Quality Improvement 3
413 - Characterizing the Neonatal Intensive Care Unit Microbiome and Evaluating the Association with Positive Blood Cultures
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 413
Publication Number: 413.1885
Publication Number: 413.1885
- MN
Mark Nolan, MD
Fellow
University of Utah
Salt Lake City, Utah, United States
Presenting Author(s)
Background: After an extended period of nearly 3 years with no central line-associated blood stream infection (CLABSI) events in the University of Utah neonatal intensive care unit (NICU), the CLABSI rate increased significantly and remains elevated. This study is part of a larger infection prevention investigation and characterizes the environmental microbiome in the NICU. It lays the groundwork for future PDSA cycles and is the baseline against which environmental microbial reduction efforts can be measured.
Objective: The objective of this study is to serve as the baseline for our ongoing quality improvement effort to reduce CLABSIs and BSIs in the NICU.
Design/Methods: Environmental samples were collected from various high-touch surfaces & equipment in the NICU, including isolettes, stethoscopes, computer workstations, and other items for 20 bedspaces in 2 high-turnover, high-acuity multi-occupancy rooms in fall 2022 and spring 2023. Samples were cultured and speciated using MALDI-TOF mass spectrometry at the Utah Public Health Laboratory. A third round of microbial sampling is currently in progress. CLABSI and BSI data were extracted from reportable Centers for Disease Control National Healthcare Safety Network data for Aug 1, 2022, through Aug 31, 2023.
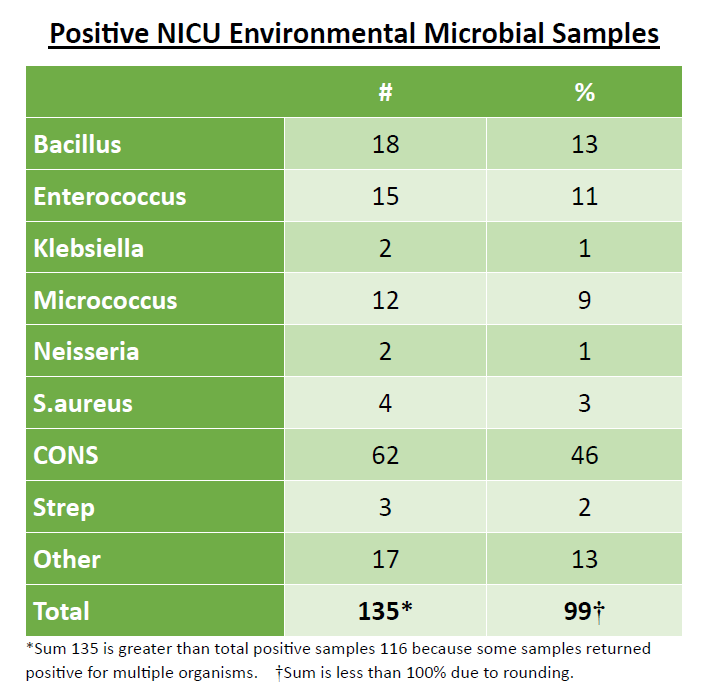
Results: A total of 461 environmental microbial samples were collected and 116 of those returned positive for 1 or more microorganisms (25% overall positivity rate). The most common microorganisms found in the NICU environment were coagulase-negative Staph, Micrococcus, and Bacillus species. S.aureus, Enterococcus, Klebsiella, and Neisseria were also found. During the study period, there were a total of 29 positive blood cultures (3 CLABSIs and 26 non-CLABSI BSIs). There was overlap between the species of microorganisms found in the NICU environment and those responsible for 21 (72%) of the total positive blood cultures including all 3 of the CLABSIs. See figures.
Conclusion(s): The overall 25% positivity rate of environmental microbial samples suggests there is a relatively high microbial burden in the NICU. Microorganisms that grew from our environmental samples were a mixture of virulent, potentially infection-causing microorganisms and those that are known to commonly colonize the environment. While a causative link cannot be concluded from the data collected, we speculate the overlap between environmental and infection-causing microorganisms responsible for positive blood cultures indicates there is a temporal and geographic association that may be contributing to the increased CLABSI rate. Further investigative and quality improvement efforts are needed.
.jpg)
