Adolescent Medicine
Session: Adolescent Medicine 2
162 - Provider Knowledge, Skills, and Attitudes in Caring for Hospitalized Adolescents with Substance Use
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 162
Publication Number: 162.159
Publication Number: 162.159
- NS
Neha S. Sharma, MD (she/her/hers)
Pediatric Hospital Medicine Fellow
Inova Fairfax Children's Hospital
Alexandria, Virginia, United States
Presenting Author(s)
Background: Overdose-related deaths in adolescents have increased, making recognition and treatment of substance use (SU) an issue of critical importance. Existing studies on provider perceptions and practices are limited to adults, outpatient pediatrics, and the mother-newborn dyad. There is limited literature in the inpatient pediatric setting.
Objective: Explore pediatric hospitalist and trainee current practices, preparedness, knowledge, comfort, and attitudes in caring for hospitalized adolescents with SU.
Design/Methods: A cross-sectional survey using a 4-point Likert scale was sent electronically to inpatient pediatric hospitalists, residents, and fellows at a large academic medical center in the mid-Atlantic region. Statistical analysis was done using the Fishers Exact Test.
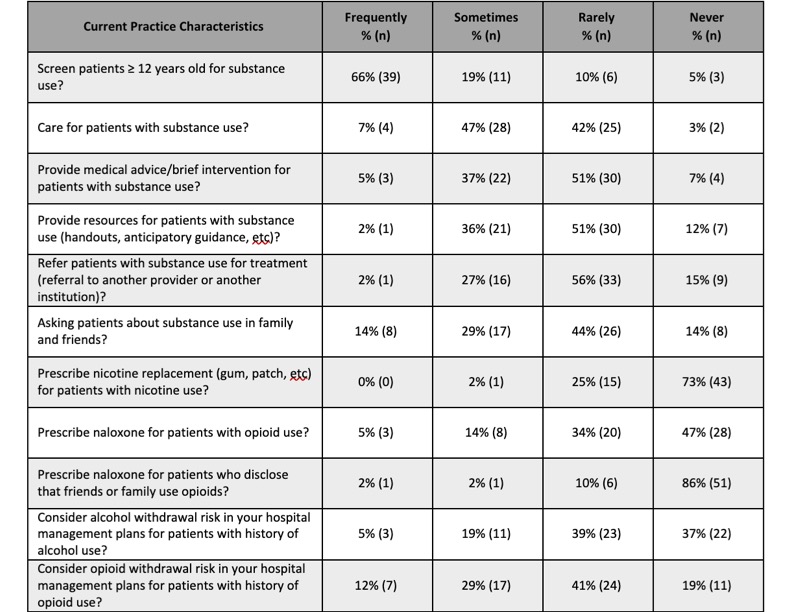
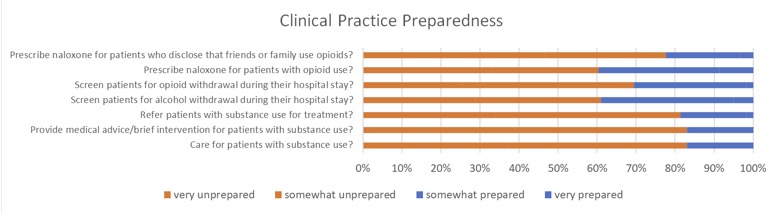
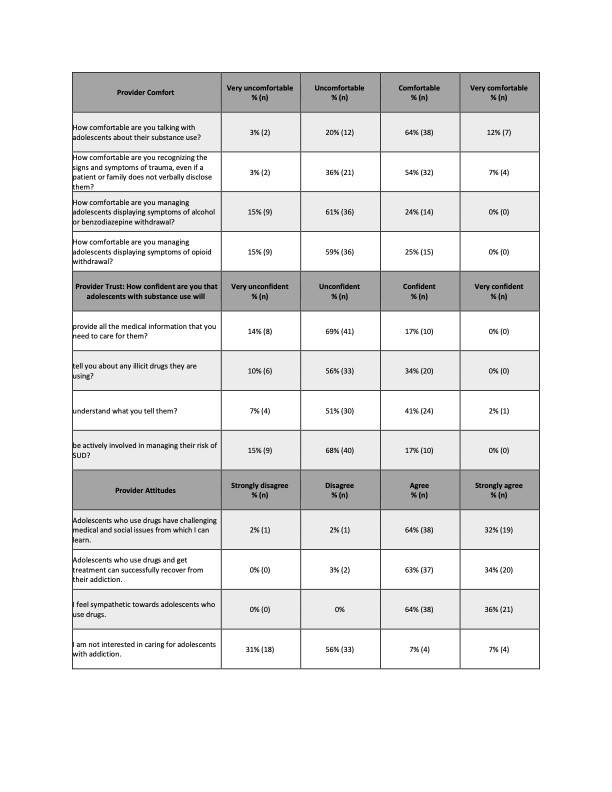
Results: 59 (81%) providers completed the survey (34, 74% trainees; 25, 93% hospitalists). Most providers (50, 85%) reported they screen adolescents for SU at least sometimes. However, trainees were more likely to screen than hospitalists (94% vs 24%, p< 0.05). Few providers (10, 17%) felt somewhat prepared to care for hospitalized adolescents with SU; none felt very prepared. Most providers reported that they rarely or never provide brief intervention (34, 58%), resources (37, 63%), or referrals (42, 71%); ask about SU in family and friends (34, 58%); prescribe nicotine replacement (58, 98%) or naloxone (48, 81%) to those at risk; and consider opioid (35, 59%) or alcohol (45, 76%) withdrawal. Of note, providers with a family history of SU were more likely to report providing a brief intervention for patients with SU (80% vs 35%, p< 0.05). Few providers agreed with having the prior training needed to provide high quality care (12, 20%) and trauma informed care (11, 19%). In addition, few have adequate knowledge to manage alcohol (9, 15%) and opioid (20, 34%) withdrawal and even fewer felt comfortable managing withdrawal (14, 24%; 15, 25%, respectively). Nearly all reported interest in receiving further training and resources for addressing adolescent SU in the inpatient setting (54, 91%). Overwhelmingly, providers felt a formal SU screening process (51, 87%) and a clinical practice guideline for recognition and management of withdrawal (55, 93%) would be beneficial for addressing SU in hospitalized adolescents.
Conclusion(s): Inpatient pediatric providers are unprepared to provide quality care for adolescents with SU. Next steps will include a quality improvement project involving the creation and implementation of a guide for screening, risk stratification, recognition, and management of withdrawal in hospitalized adolescents with SU.