Neonatology
Session: Neonatal Quality Improvement 4
62 - Improving the home ventilator transition process in a level IV Neonatal Intensive Care Unit
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 62
Publication Number: 62.3225
Publication Number: 62.3225
.jpeg.jpg)
Parul Cham, DO (she/her/hers)
Clinical Assistant Professor of Pediatrics
University of Michigan Medical School
Ann Arbor, Michigan, United States
Presenting Author(s)
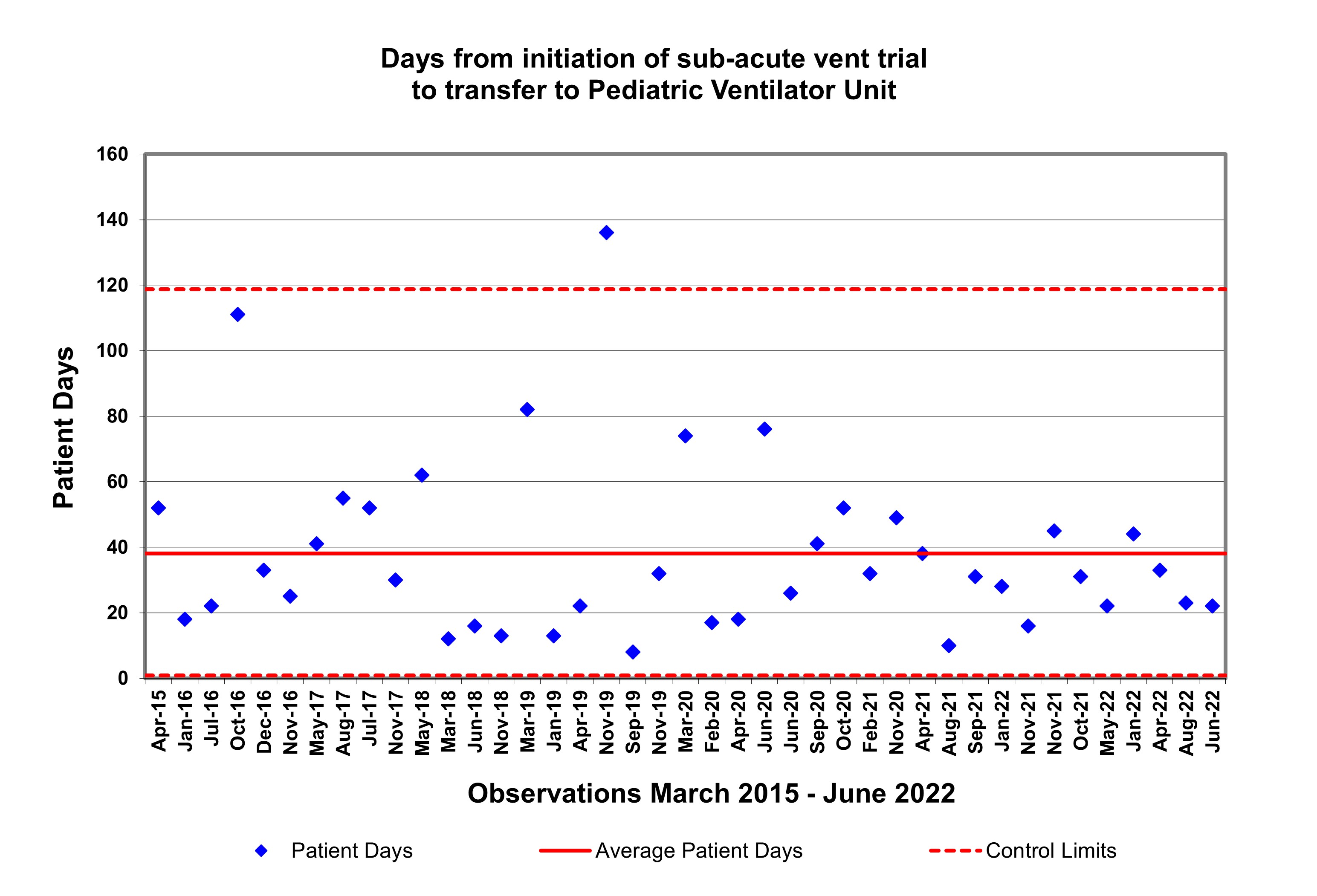
Background: Transition from hospital ventilator to home ventilator is a necessary step towards discharge for long-term ventilated patients. It is a complicated process that is based on patient disease characteristics, patient readiness and the transition practices of the unit. It is associated with high hospital costs due to prolonged hospitalization. Systems-based processes specific to home ventilator transition in the Neonatal Intensive Care Unit (NICU) have not been well standardized. Baseline assessment of home ventilator transition process at the University of Michigan identified a high degree of variability with a mean time of 39 days (range 12-111) from initiation of home ventilator to transfer to pediatric ventilator unit (PVU) (Figure 1) and an average total hospital length of stay of 196 days. This prompted the creation of a quality improvement initiative to improve the home ventilator transition process and impact length of stay.
Objective: Reduce the time from initiation to transfer to the PVU and decrease hospital length of stay for NICU patients requiring tracheostomy and home ventilator via a home ventilator transition bundle.
Design/Methods: A multidisciplinary team of nurses, nurse practitioners, physicians, and respiratory therapists from the NICU and the PVU was established to identify key steps and barriers in the transition to home ventilator. Baseline surveys were distributed to all NICU staff to better understand the transition process from different perspectives. Survey results and process mapping identified key drivers for improvement (Figure 2). Using QI methodology, small tests of change were used to develop standardized criteria for readiness for of home ventilator trials followed by the creation of a novel scoring tool assessing trial tolerance, a standardized process for intervention based on scoring and a process for documentation of trials. Days from first initiation of home ventilator trial to the PVU was tracked by a control chart as a key outcome measure.
Results: Baseline data revealed a chaotic process with multiple patient- and process-level factors impacting transition. The implementation of standardized readiness criteria, a scoring tool, and score-based intervention guideline resulted in fewer outliers (Figure 3) in the transition process without increase in length of stay.
Conclusion(s): Given the rarity of this process, more data over time is required to signal meaningful change though our data are encouraging. The creation, continued implementation and measurement of our bundle, we demonstrate steps to improve the transition to PVU and decrease hospital length of stay.
.jpg)
.jpg)
