Clinical Bioethics
Session: Clinical Bioethics
430 - Nurses' experiences influence opinions on the ethical use of pediatric dialysis
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 430
Publication Number: 430.1807
Publication Number: 430.1807

Carly Eiduson (she/her/hers)
Medical Student
University of Rochester School of Medicine and Dentistry
Rochester, New York, United States
Presenting Author(s)
Background: Advances in pediatric dialysis have led to improved outcomes for patients. There is debate whether pediatric renal replacement therapy (RRT) is morally obligatory, leading to ethical issues surrounding decision making. While the physician may be the primary decision-making co-partner with families considering RRT, bedside nurses spend a lot of time with patients on dialysis.
Objective: To better understand bedside neonatal, pediatric, and pediatric cardiac ICU nurses’ beliefs regarding the ethics of pediatric RRT.
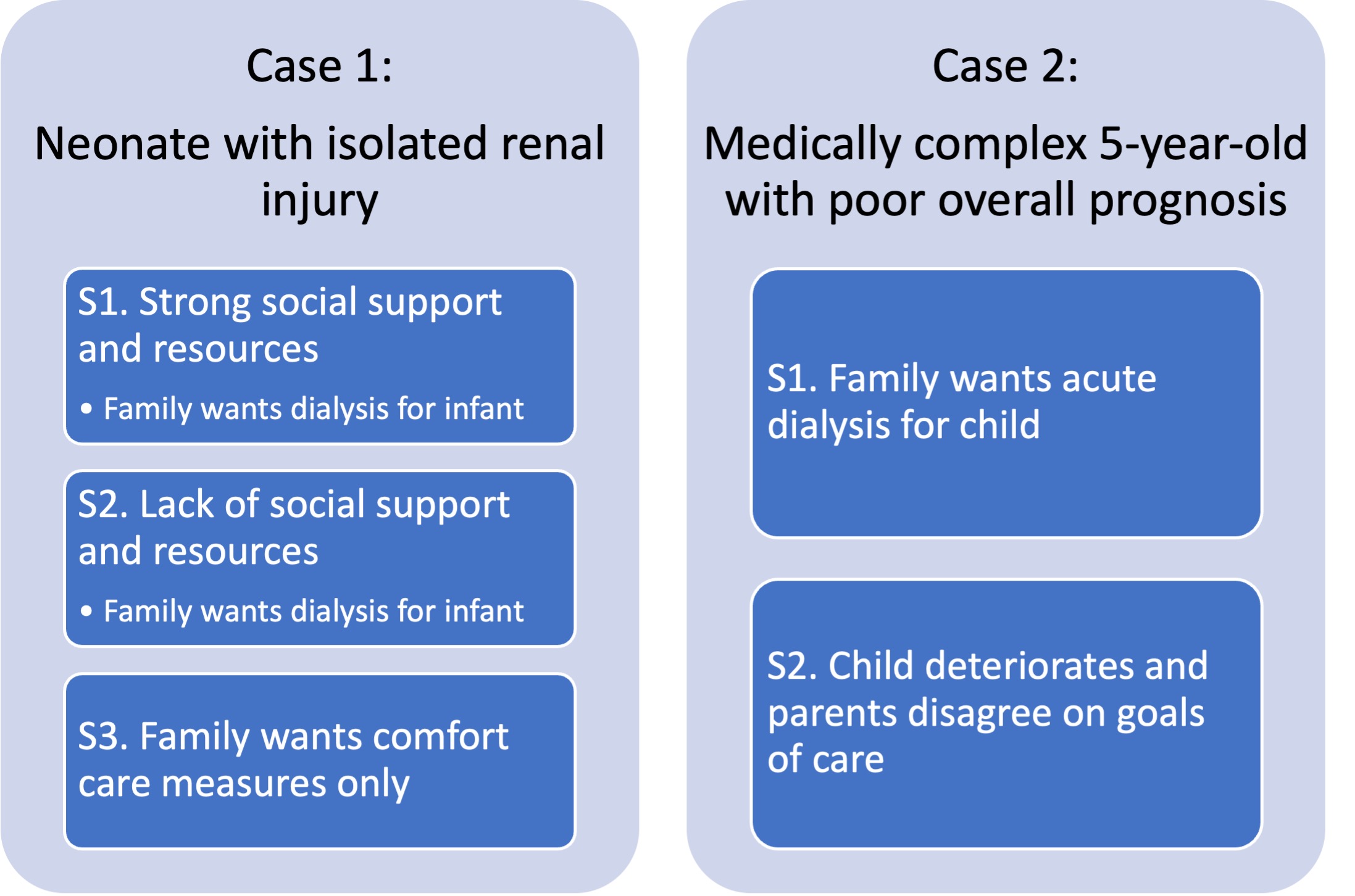
Design/Methods: This is a single-center case scenario survey study. A REDCap survey was disseminated to nurses in the neonatal, pediatric, and pediatric cardiac intensive care units at Golisano Children’s Hospital. The survey included four sections: (1) demographics, (2) decision making and ethics related to advanced therapies, (3) two multi-part case-based scenarios (Figure 1), (4) additional related questions. Survey outcomes were compared among nursing cohorts using Wilcoxon Rank Sum tests or Chi-Squared/Fisher’s exact tests, where appropriate.
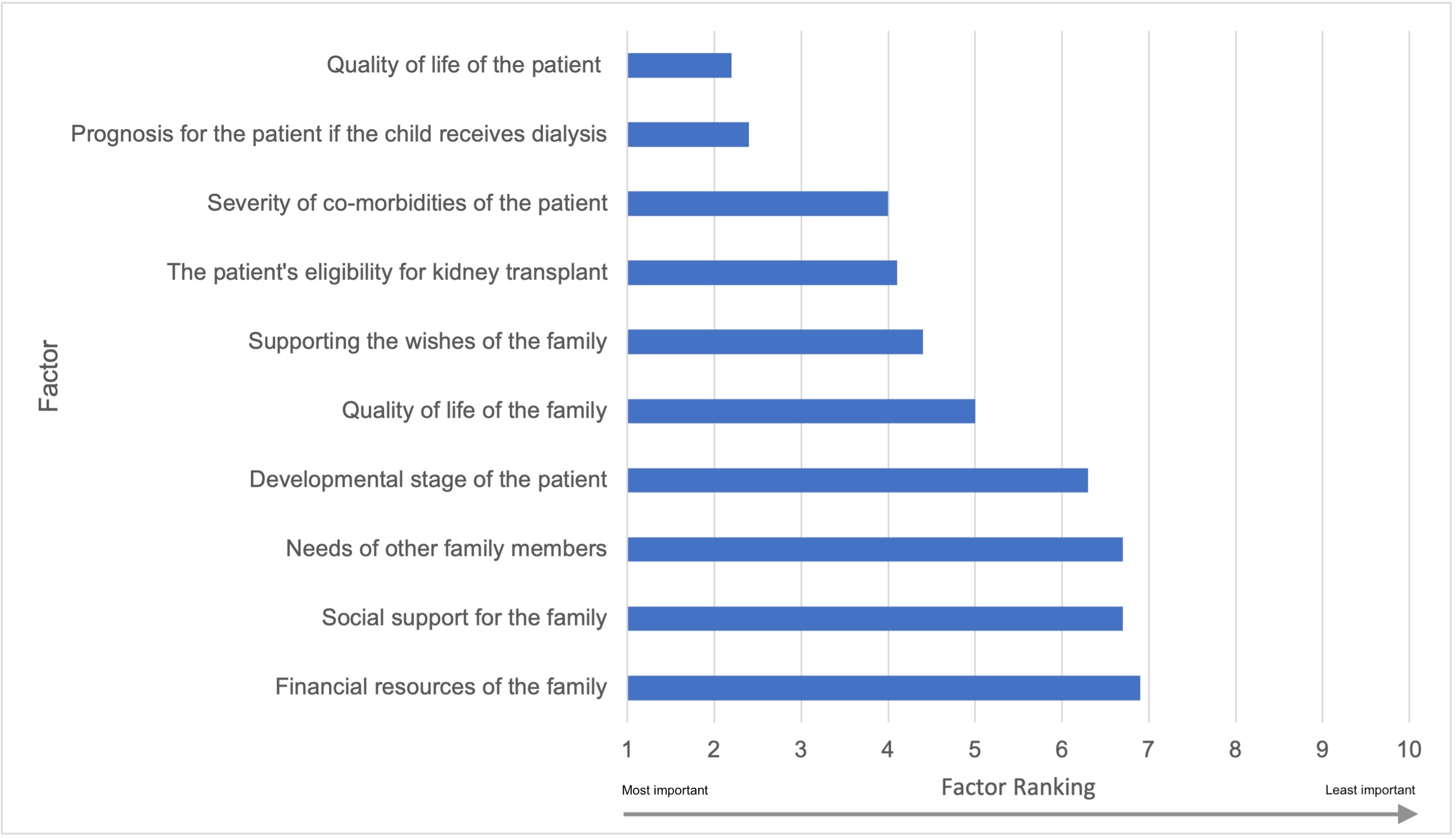
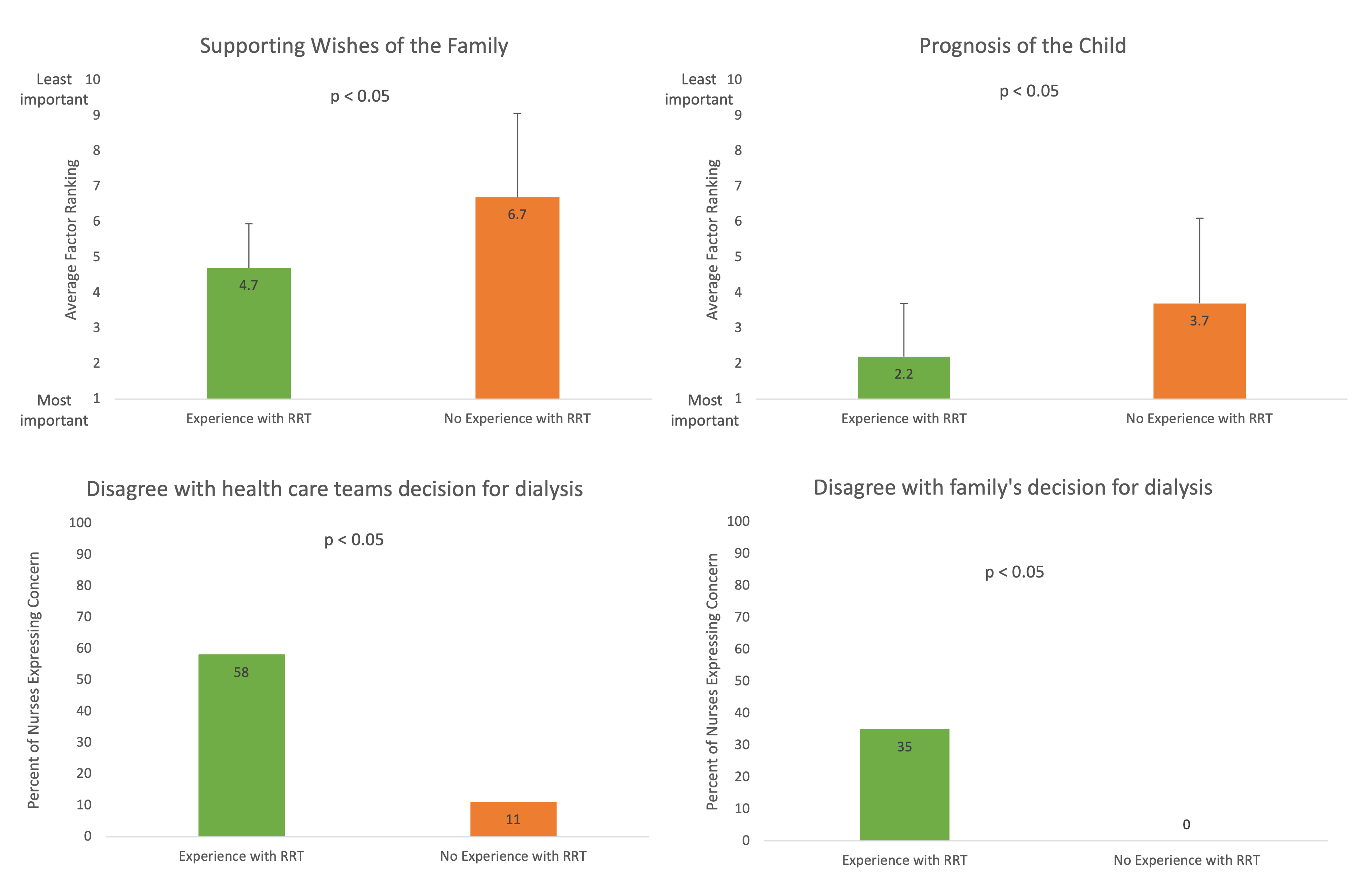
Results: 63 nurses (20 NICU, 5 PICU, 9 PCCC, and 2 working in > 1 unit) completed at least part of the survey; 36 completed all parts. The respondents identified as majority white and between 31-50 years old; most with ≥2 years of ICU experience, with 1/4 with ≥20 years; around 3/4 had experience caring for a child on RRT. The most important factors influencing nurses’ opinion of appropriateness of RRT were patient quality of life (QoL), patient prognosis, and severity of co-morbidities (Figure 2). QoL was more important to nurses with more years of nursing experience (ρ=0.33, p =0.023). Nurses with experience caring for patients on RRT deemed patient prognosis (2.2+/- 1.3 vs. 3.7 +/- 2.4 p=0.027) and family wishes (4.7+/- 2.4 vs. 6.7 +/- 1.3 p=0.042) more important than did nurses without RRT experience (Figures 3a, 3b). Dependent on case scenario and RRT experience, nurses reported varying responses to what action they would take if they disagreed with a decision to pursue RRT, but nurses with RRT experience were more likely to favor expressing their concern to the team/family (Figures 3c, 3d). 86% of respondents believe there is a moral obligation to offer RRT and 33% believe there is a moral obligation to initiate RRT for medically appropriate patients.
Conclusion(s): The decision to treat with RRT is not limited to medical eligibility. Our survey reveals bedside nurses approach patient care through a biopsychosocial lens. Future investigation is needed on the opinions of healthcare team members including medical trainees, residents, and fellows.