Children with Chronic Conditions
Session: Children with Chronic Conditions 1
263 - Prevalence of Mental and Behavioral Health Diagnoses in Children with Medical Complexity
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 263
Publication Number: 263.161
Publication Number: 263.161
.jpg)
Kristina Malik, MD (she/her/hers)
Assistant Professor
University of Colorado School of Medicine
Aurora, Colorado, United States
Presenting Author(s)
Background: Children with special health care needs (CSHCN) have higher rates of mental and behavioral health (MBH) diagnoses than children without special healthcare needs. Children with medical complexity (CMC), a subgroup of CSHCN with serious medical conditions and resulting functional limitations, are at higher risk for MBH disorders and have reported barriers to MBH care specific to their complexity status, but the rates of MBH diagnoses have not been well described.
Objective: To compare mental and behavioral health status between CMC and CSHCN using a nationally representative sample.
Design/Methods: Cross-sectional analysis of annual data from the 2016-17 National Survey of Child Health. CMC and CSHCN were identified using validated algorithms. The primary outcome was MBH status, as measured by a child’s caregiver-reported occurrence of a MBH diagnosis (anxiety, depression, behavioral or conduct problems, substance abuse, ADHD, other); secondary outcomes included MBH service and medication use and need. Bivariate analyses compared the prevalence of the MBH status and service use by medical complexity status. All statistics accounted for the complex survey design.
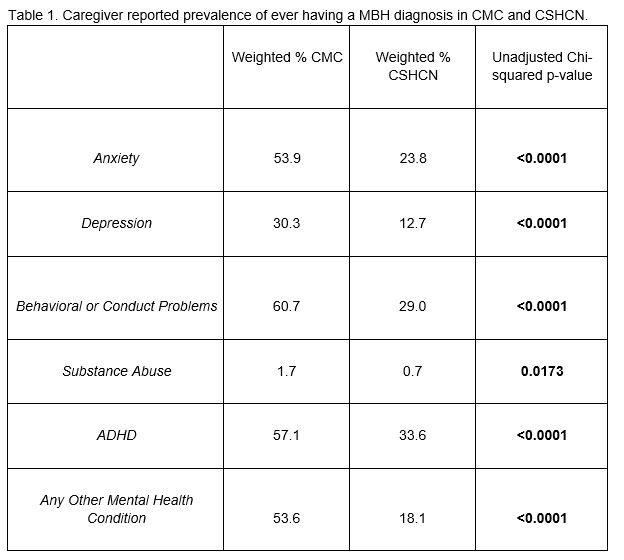
Results: Of 15,518 CSHCN ages 3–17 years, 7.2% were CMC and 92.8% were “non-CMC” CSHCN. CMC were 2 times more likely than CSHCN to have any specific MBH diagnosis (p ≤ 0.017 for all, table 1). Anxiety, behavioral or conduct problems, and ADHD were each reported in over half of CMC. CMC, with and without MBH diagnoses, were more likely to receive treatment or counseling from a mental health professional than CSHCN (64.4 v 29.2%, p< 0.001) or take medication for their difficulties with emotions, concentration, or behavior (59.8 v 29.2, p< 0.001) in the past year. Eleven percent of CMC and 6.2% CSHCN reported not being able to see a mental health professional when needed over the past year (p=0.026). Of children who saw or needed to see a mental health profession in the past year, 25.5% of CMC and 15.8% of CSHCN reported getting the needed treatment and counseling was a big problem (p=0.005).
Conclusion(s): In this study, over half of CMC had a mental and behavioral health diagnosis. CMC have higher prevalence of MBH disorders than non-CMC CSHCN, have higher MBH service and medication use, yet reported higher rates of not being able to access MBH care or high level of difficulty accessing MBH care. Taking these findings in context of prior reported barriers to MBH care specifically experienced by CMC can help prioritize next steps in improving MBH outcomes for CMC.