Infectious Diseases
Session: Infectious Diseases 1
578 - Follow up Care of Multisystem Inflammatory Syndrome in the Pediatric Population of the Military Healthcare System
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 578
Publication Number: 578.162
Publication Number: 578.162
- AS
Apryl Susi, MS, MLS (ASCP)CM (she/her/hers)
Clinical Epidemiologist III
HJF/USUHS, GWU
Bethesda, Maryland, United States
Presenting Author(s)
Background: The CDC describes Multisystem Inflammatory Syndrome (MIS) as an immune mediated disease associated with COVID-19 in which various body parts become inflamed including the heart, lungs, brain, kidneys, eyes, skin, and gastrointestinal tract. Little is known about outcomes after initial MIS diagnosis.
Objective: To describe trends of MIS, the patient population, complications, and follow-up care of children and young adults 0-21 years of age in the US Military Health System (MHS).
Design/Methods: A retrospective study was conducted using the MHS data repository to investigate incident inpatient encounters with an ICD-10 code for MIS Jan 2021 through Aug 2022, describe trends, co-occurring diagnoses and procedures, demographic characteristics, and care patterns following discharge.
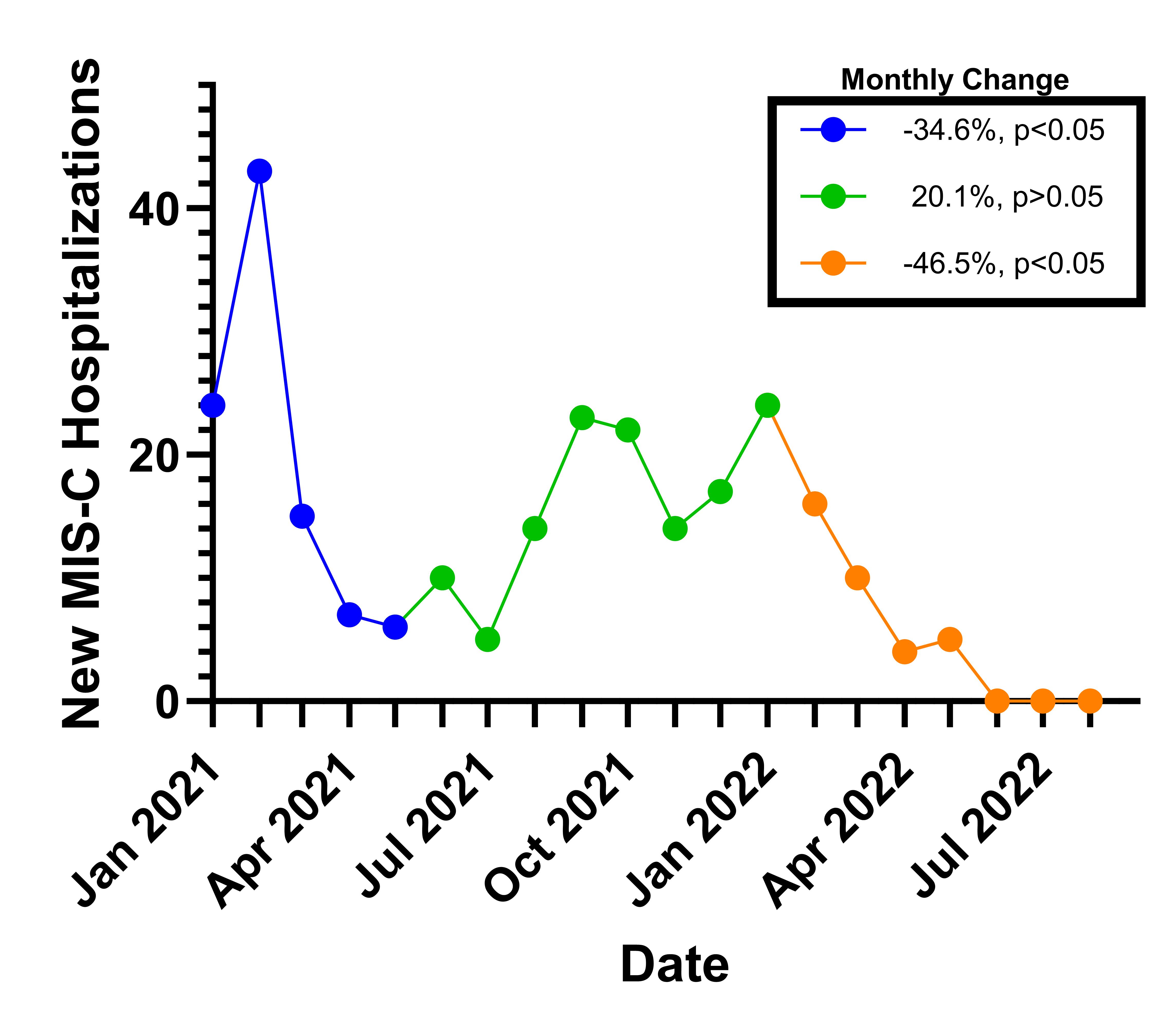
Results: There were 261 incident inpatient encounters for MIS that decreased monthly from Jan 2021 to May 2021, had a non-significant increase from May 2021 to Jan 2022, before decreasing again from Jan 2022 to Aug 2022(Figure 1).
Those hospitalized with MIS were mostly male (62%), dependents (87%), resided in the south (39.5%), and had a median age of 8 (IQR 4-12) years. 47% of inpatient stays included intensive care, and the median hospital length of stay was 5 days (IQR 4-7), with a range of 1-63 days.
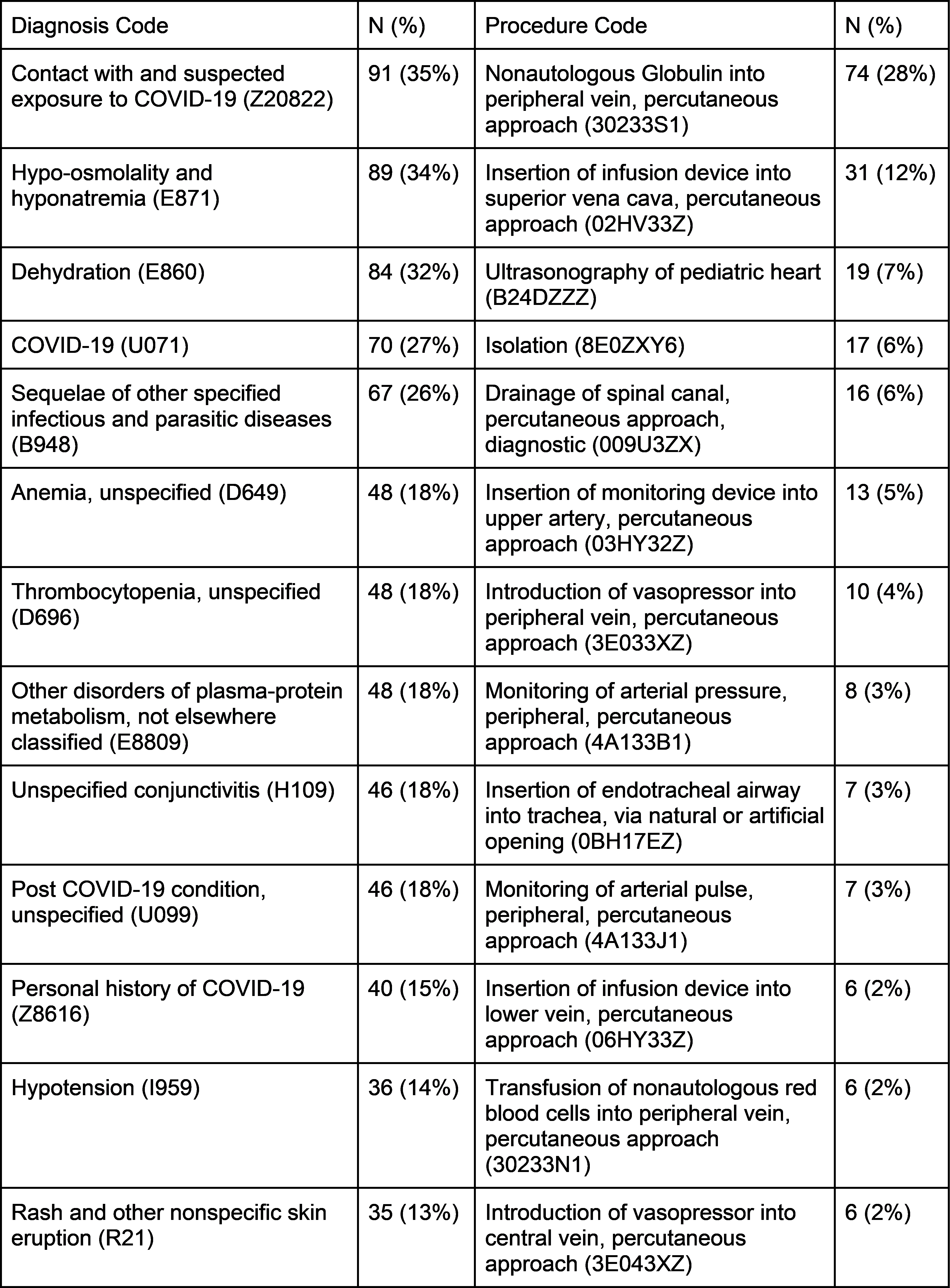
The most common complications of MIS were hypo-osmolality and hyponatremia (34%), dehydration (32%), anemia (18%), thrombocytopenia (18%), other disorders of plasma-protein metabolism (18%), and conjunctivitis (18%). The most common procedure was administration of intravenous immunoglobulin (28%)(Table 1).
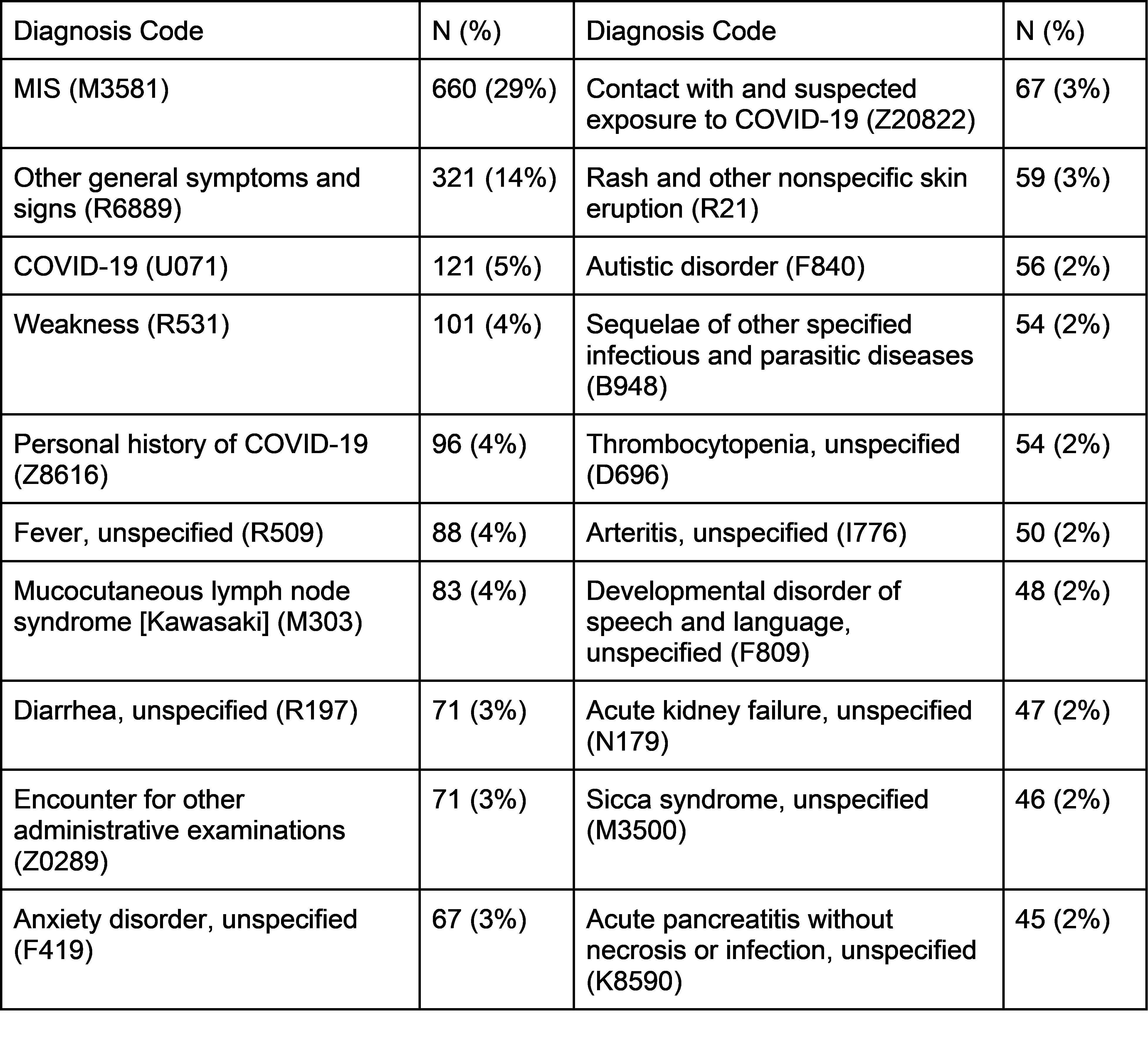
In the 90 days following their initial MIS inpatient discharge, 16 (6.1%) had a hospital admission. In the same period, 254 (97.3%) had at least one outpatient encounter, with a median of 6 (IQR 4-10) encounters, for a total of 2,309 encounters. Outpatient care was largely recorded as MIS and COVID follow-up; weakness (4%), fever (4%), Kawasaki disease (4%), anxiety (3%) and rash (3%) were also key diagnoses following MIS hospitalization(Table 2).
Conclusion(s): The trends experienced in the MHS are similar to those documented by the CDC suggesting validity of the ICD-10 record. The most common co-occurring diagnoses corresponded to key clinical diagnostic features of MIS. Serious complications of MIS and invasive procedures are relatively common, such as acute kidney failure, and nearly half of the patients required ICU admission. Given the high intensity of healthcare utilization after discharge, case management may be helpful. Longer-term outcomes beyond 90 days of MIS should be explored.