Hospital Medicine
Session: Hospital Medicine 3
332 - Community Hospital Rotations: National Survey of Pediatric Hospital Medicine Fellowship Program Directors’ Perspectives
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 332
Publication Number: 332.163
Publication Number: 332.163

My-Linh Ngo, MD (she/her/hers)
Assistant Professor of Clinical Pediatrics
Monroe Carell Jr. Children's Hospital at Vanderbilt
Nashville, Tennessee, United States
Presenting Author(s)
Background: A community hospital medicine rotation is required by Accreditation for Graduate Medication Education (ACGME) in Pediatric Hospital Medicine Fellowship (PHMF). However, community-based pediatric inpatient care is diminishing as the economic impact of maintaining rural hospitals increases. Therefore, the challenge increases for Program Directors (PDs) to find and create partnerships with community sites for their training experiences. No studies have evaluated PDs’ perspectives on this requirement.
Objective: To assess program directors’ perspectives on creating and maintaining pediatric community hospital rotations.
Design/Methods: We surveyed national PHMF PDs using an online REDCap survey. Survey items were generated after literature review and with iterative input from experts in PHM training and community-hospital medicine leaders. The survey was piloted with PHMF Associate PDs for additional revisions before dissemination to PHMF PDs. The 42-item survey queried PHMF program demographics; establishment of community hospital partnerships; community hospital characteristics; PD satisfaction with site characteristics [5-pt scale (1=not at all, 5=extremely)]; ACGME accreditation; and ACGME citations related to the community rotation. Descriptive statistics and Fisher’s exact test were used for analyses.
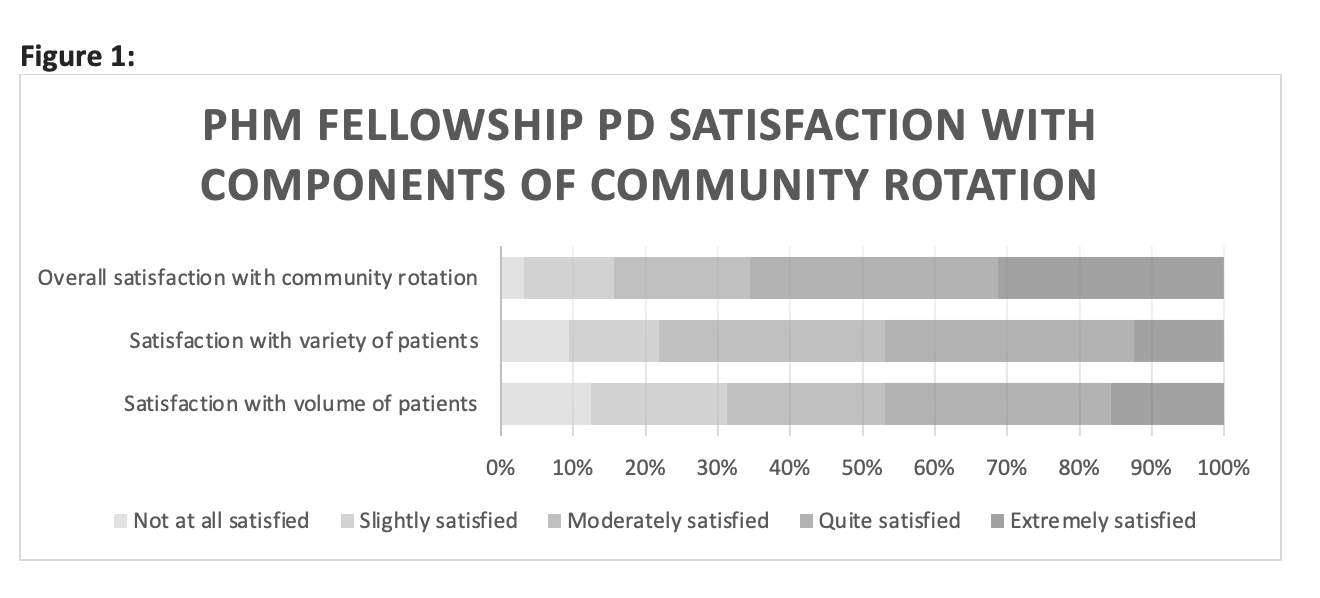
Results: Thirty-eight PDs completed the survey (response rate: 52%), representing programs in 9 regions in the US and Canada. Of respondents, 84% (32 programs) established a community partnership. For 38% (12/32) of these, more than one community partnership was needed. Most community sites provided dedicated inpatient care 88% (28/32). Commutes ≥91 minutes were necessary for 9% (3/32). Although PDs reported low satisfaction with volume (31%, 10/32) and patient variety (22%, 7/32) at their community site, 66% (21/32) of PDs were more satisfied with their overall rotation experience (Figure 1). Of the 38 respondents, 92% (35) were ACGME-accredited programs. Of those who were ACGME-accredited, 11% (4) received a citation related to their community site. No statistical significance was noted in analyzing responses for identifying community sites nor rotation satisfaction between programs with and without an ACGME citation.
Conclusion(s): We identified national variability in PHMFs’ ability to find community sites and establish community partnerships and in community hospital characteristics. Future directions include analyzing the impact of diminishing pediatric community inpatient care on fellow education. It may become necessary for this ACGME requirement to be revised.