Health Equity/Social Determinants of Health
Session: Health Equity/Social Determinants of Health 5
274 - Perceptions of Social Determinants of Health Screening and Resource Connection in Families Recently Discharged from a Pediatric Hospital
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 274
Publication Number: 274.1676
Publication Number: 274.1676

Ashley A. Hollo, MD, MPH (she/her/hers)
Resident
University of Colorado
Denver, Colorado, United States
Presenting Author(s)
Background: Social determinants of health (SDOH) have a significant impact on the health and development of children. Thus, hospitals should consider screening for SDOH and referring to community-based organizations to provide more comprehensive care. While several studies have evaluated screening outcomes during hospitalization, few have evaluated families’ perceptions of screening and connection to community resources following discharge.
Objective: To examine patient and family perceptions of SDOH screening and factors associated with families’ connection to socio-economic resources after pediatric hospital discharge.
Design/Methods: A post-discharge phone survey was conducted of families who had been screened during their child’s admission to a free-standing children’s hospital. Families were screened on six social needs (SN) categories: 1) financial concerns, 2) keeping appointments, 3) filling prescriptions, 4) food insecurity (FI), 5) benefits, and 6) housing insecurity. Screen-positive families were offered community-based referrals and resources during the hospitalization. Phone surveys were conducted two weeks post-discharge to assess parents’ perceptions of SN screening, connection to resources, and perceived helpfulness of these resources. Demographic and screening characteristics were compared between families who reported connecting or not connecting to resources using Pearson’s chi-square, Fishers Exact, or Wilcoxon Rank Sum tests.
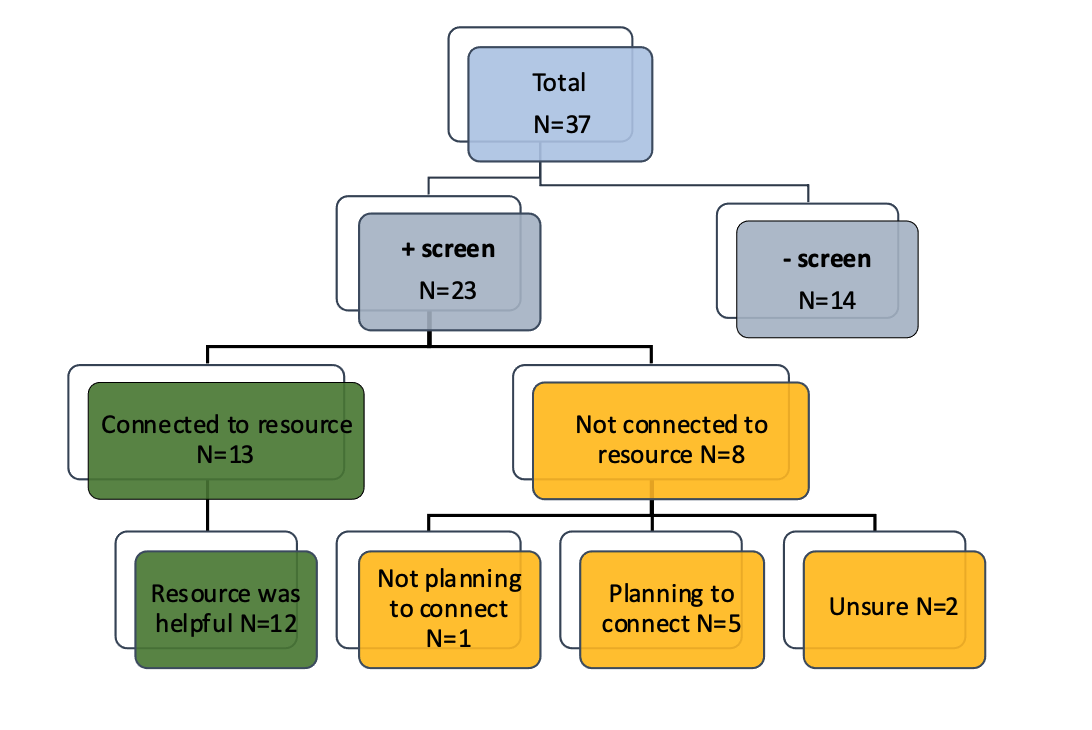
Results: Out of 37 families surveyed post-discharge, 23 (62%) had a positive SDOH screen during the hospitalization. Of these, 13 (56%) reported connecting to community resources after discharge, while 8 (35%) did not connect, and 2 (9%) did not disclose. Twelve (92%) of the 13 families that reported connecting to resources found them to be helpful. Five (62%) of the eight families not connected were still planning to do so (Fig 1). Respondents’ perceptions of SDOH screening are shown in Table 1. Families reporting a connection to resources screened higher for positive SNs (3 vs. 1; p=0.01) and were more likely to screen for FI (54% vs. 0%; p=0.018) during hospitalization than families who reported not connecting to resources (Table 2).
Conclusion(s): Despite a small sample size, our results indicate that most families find inpatient SDOH screening and resource referral to be acceptable and beneficial. Certain screening characteristics may correlate with post-discharge linkage to resources, though further study is needed to explore why families may not connect with offered resources.
.png)
.png)
