Neonatology
Session: Neonatal Quality Improvement 5
84 - Minimally Invasive Surfactant Therapy (MIST) Implementation in Comer NICU
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 84
Publication Number: 84.3333
Publication Number: 84.3333
Natasha Ahn, MD MPH (she/her/hers)
Neonatology Fellow
Comer Children's Hospital at University of Chicago Medical Center
Chicago, Illinois, United States
Presenting Author(s)
Background: Historically intubation and positive pressure ventilation (PPV) has been the only way to deliver surfactant to neonates with respiratory distress syndrome (RDS); however, minimally invasive surfactant therapy (MIST) using a thin catheter technique eliminates the need for intubation and PPV. There is increasing evidence that MIST is associated with favorable outcomes, including reduction in need for invasive mechanical ventilation (MV), death and/or bronchopulmonary dysplasia (BPD).
Objective: Measure implementation and effectiveness of introducing MIST at a single center NICU. Primary implementation outcome is percentage of infants who receive MIST vs the previous standard of care intubation-surfactant-extubation (InSurE) over 1 year after implementation. Primary efficacy outcome is rate of intubation within 7 days of surfactant in patients who receive MIST vs InSurE.
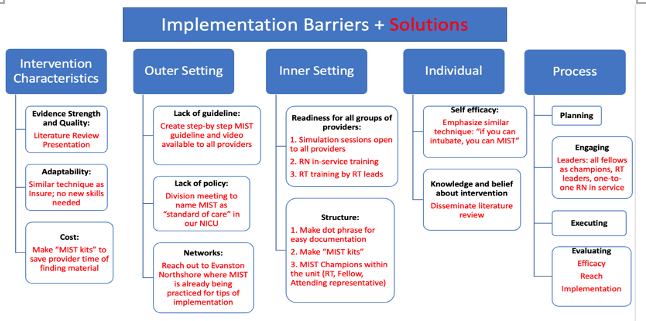
Design/Methods: MIST was implemented in June 2023 into a 71 bed Level IV NICU that had previously been using InSurE as standard of care for infants who did not require immediate intubation and ventilation. Implementation strategy is outlined in Figure 1. All patients eligible for InSurE were eligible for MIST. Detailed chart review of all patients who received minimally invasive surfactant since June 2022 was performed to measure predetermined implementation and efficacy outcomes.
Results: Since June 2022, 37 patients were administered surfactant (Poractant Alpha) via InSurE and 25 via MIST. There were no significant differences in mean gestational age, birth weight, amount of respiratory support and timing at which infants in each group received first dose of surfactant (Table 1). The primary implementation outcome was significant: 96% (p= < 0.001) of infants eligible for surfactant received it via MIST after implementation (Table 2). The primary efficacy outcome was not significant: 19% of infants who received InSurE got intubated <=7 days vs 17% of infants who received MIST (p=0.63) (Table 2). Of note, there was a significant decrease in FiO2 after 1 hr in MIST compared to InSurE, but this difference was not significant 4 and 24 hours post surfactant.
Conclusion(s): MIST was effectively implemented into Comer NICU: 96% of infants who needed minimally invasive surfactant received it via MIST. The sample size is still too small to detect a significant improvement in efficacy, but this preliminary data shows a promising trend in decreasing intubation rates and weaning off oxygen quicker. Next, secondary outcomes (BPD, IVH, NEC, ROP, air leak) will be collected for infants who received MIST and InSurE.
.png)
.png)
