Health Equity/Social Determinants of Health
Session: Health Equity/Social Determinants of Health 7
297 - Investigating Re-traumatization Risk With ACEs Screening and Pediatrician-led Discussions Among Hispanic Caregivers
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 297
Publication Number: 297.1697
Publication Number: 297.1697

Chiara M. Bettale, BA, MD candidate (May 2024) (she/her/hers)
Medical Student
Emory University School of Medicine
Decatur, Georgia, United States
Presenting Author(s)
Background: Screening for adverse childhood experiences (ACEs) allows for healthcare providers to mitigate negative intergenerational impacts on health outcomes. However, there remains concern about the potential harmful effects of ACEs screening and discussion on psychological health through re-traumatization. The direct effect of ACEs screening on posttraumatic stress symptoms (PTS) has yet to be studied.
Objective: To determine if screening or provider-led discussion of parental ACEs are associated with inadvertent worsening of PTS 1 week after screening.
Design/Methods: Providers in a pediatric primary care clinic serving predominantly Hispanic and low socioeconomically resources families in an urban setting were randomized to an intervention group or standard of care. Providers in the intervention group received a 4-hour training on provision of a trauma-informed discussion on the impact of ACEs on parenting. Then, caregivers attending 4-, 6-, 9-, 15-, or 18-month well child checks completed by any provider in the clinic completed a 10-item ACEs questionnaire and post-traumatic stress disorder (PTSD) screen for DSM-5 (PC-PTSD-5). Participants completed repeat PTS survey measures one week later. Paired and Welch Two sample t-tests were conducted to detect within and between-group changes in PTSD symptoms 1-week after ACE screening.
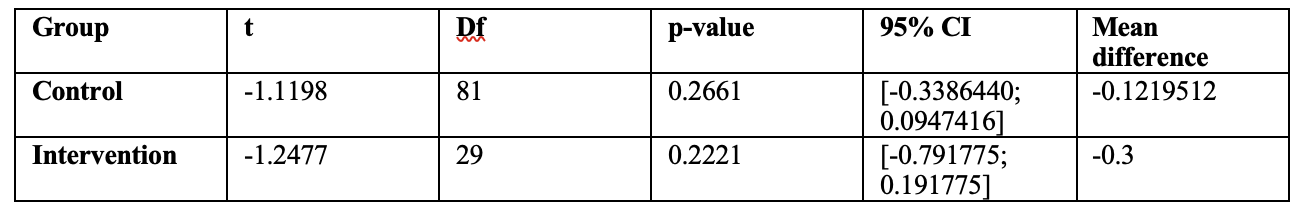
Results: Out of 142 enrolled participants, 112 completed both baseline and 1-week measures (Table 1 shows demographic data). Nine percent of the sample (n=10) screened positive for PTSD (score ≥ 3), demonstrating the presence of clinically significant PTS within this sample. Mean ACE score was 2.52 (SD 2.31, 95% CI [2.10; 2.95]); 78% of the study participants experienced at least one ACE and 30% experienced ≥ 4 ACEs, which is in line with national data. Paired t-test analysis in the overall sample showed no significant change in PTSD scores 1-week after ACEs screening (t(111) = 1.660, p = .10, 95% CI = [-0.03, 0.37]) with no PTSD score changes within the control and the intervention groups (Table 2). Welch Two sample t-test also showed no significant change in 1-week PTSD scores between groups, t(47.992) = 0.243, p = .81, 95% CI = [-0.40, 0.51].
Conclusion(s): Screening and trauma-informed discussion of ACEs with trained providers were not associated with worsening PTS symptoms in this sample. This suggests that screening and discussion of ACEs can be safely administered in pediatric primary care settings. This may mitigate provider hesitancy of implementation of ACEs screening when adequate resources and referrals are in place.
.png)