Neonatology
Session: Neonatal Quality Improvement 2
405 - Provision of breast milk after implementation of a breast milk tracking system
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 405
Publication Number: 405.1701
Publication Number: 405.1701
.jpg)
Elisabeth Romero, MD (she/her/hers)
Pediatric Resident
Baystate Children's Hospital
Springfield, Massachusetts, United States
Presenting Author(s)
Background: Breast milk (BM) is critical to optimizing health outcomes for all infants. Those admitted to the Neonatal Intensive Care Unit (NICU) commonly experience barriers to BM feeding. BM provision issues are common due to parent-infant separation, inadequate volumes, and lack of support. BM safety errors, including handling, mixing and feeding mishaps, can also occur in the NICU setting. Breast milk tracking systems with an app-based parent communication interface (BMTS) can be implemented to help decrease BM errors and improve parental communication and support.
Objective: To evaluate whether implementation of a BMTS improves provision of BM for infants at discharge from a level III NICU.
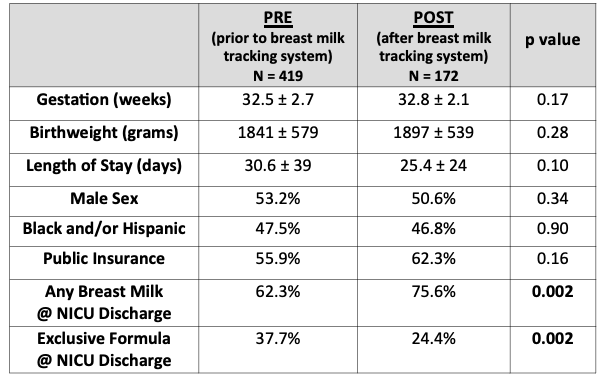
Design/Methods: A retrospective cohort study was conducted on all surviving infants discharged home from the NICU over a 2-year period. The first cohort was pre-BMTS implementation (PRE: Jan 2021 – March 2022) and the second cohort was post-BMTS implementation (BMTS: April 2022 - Dec 2022). Infant characteristics such as feed-type at ultimate discharge (primary outcome), gestational age (GA), birthweight (BW), and length of stay (LOS) were collected. Parental-NICU communications and BM error rates were estimated by staff. Descriptive statistics were computed and comparisons made by Chi-squared test/Fisher’s exact test and student t test as appropriate (significance p< 0.05).
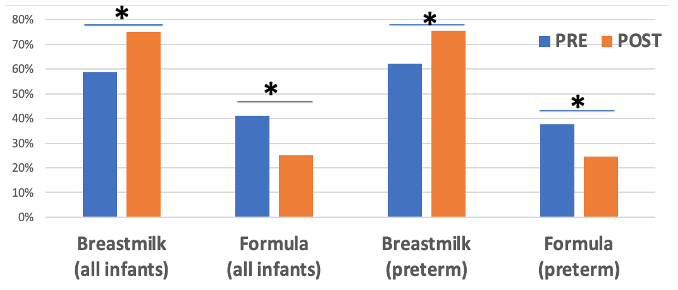
Results: A total of 2,344 infants qualified for this study (PRE cohort: n= 1,831; and BMTS cohort: n = 513) with an average GA of 35 weeks and BW of 2.6 kg. There were no differences in GA, BW and LOS between cohorts. As compared to the PRE cohort, the BMTS cohort saw an improvement in discharge BM provision from 58.8% to 75% and a decrease in exclusive formula use from 41.2% to 25% (p < 0.001). Results were similar when comparing a subset of only preterm infants < 35 weeks’ gestation: 61.9% in the PRE subset (n=712) and 75.6% in BMTS subset (n= 172) received any BM ay NICU discharge with a concordant drop is formula use (p < 0.001). The BMTS cohort also had estimated less BM errors and increased parental-NICU communications.
Conclusion(s): The implementation of a BMTS in a level III NICU has been associated with increased BM provision and less exclusive formula use at discharge. The increased parental communications using the BMTS-parent interface and the perceived decrease in BM errors may have contributed to the overall improvement in BM provision.