Hospital Medicine
Session: Hospital Medicine 1
308 - Hemoglobin threshold and blood transfusion in young children hospitalized with iron deficiency anemia
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 308
Publication Number: 308.18
Publication Number: 308.18
.jpg)
Doulin (Rose) Sun, MD FRCPC FAAP (she/her/hers)
Trainee
University of Toronto Temerty Faculty of Medicine
Calgary, Alberta, Canada
Presenting Author(s)
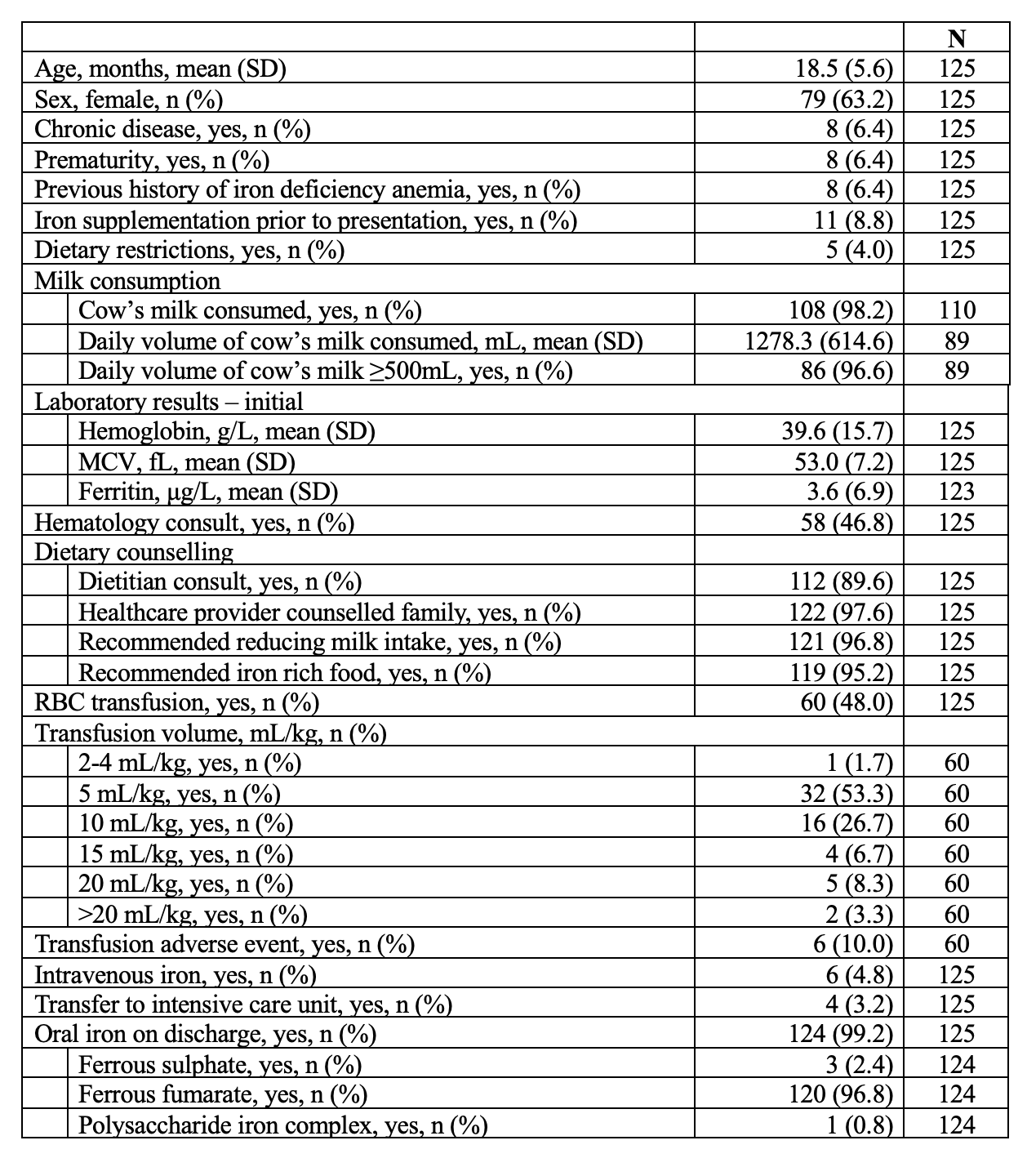
Background: In 2022, the American Society of Pediatric Hematology/Oncology published Choosing Wisely recommendations, advising against red blood cell transfusion in asymptomatic children with IDA and no evidence of hemodynamic instability or active bleeding. However, the guideline does not provide a hemoglobin threshold for transfusion or criteria for hemodynamic instability.
Iron deficiency anemia (IDA) peaks in prevalence in early childhood and may be associated with heart failure, cerebral thrombosis and impaired cognitive function. Therefore, timely detection and treatment are important to minimize poor health outcomes. Examination of real-world transfusion practice in children hospitalized with severe IDA may help inform resource stewardship efforts, including the implementation of Choosing Wisely recommendation.
Objective: Current recommendations advise against transfusion of red blood cells (RBC) in asymptomatic children with iron deficiency anemia (IDA) and no evidence of hemodynamic instability; however, little is known about real-world practice. Our objective was to determine predictors of transfusion, specifically hemoglobin level and measures of hemodynamic instability, in young children hospitalized with IDA.
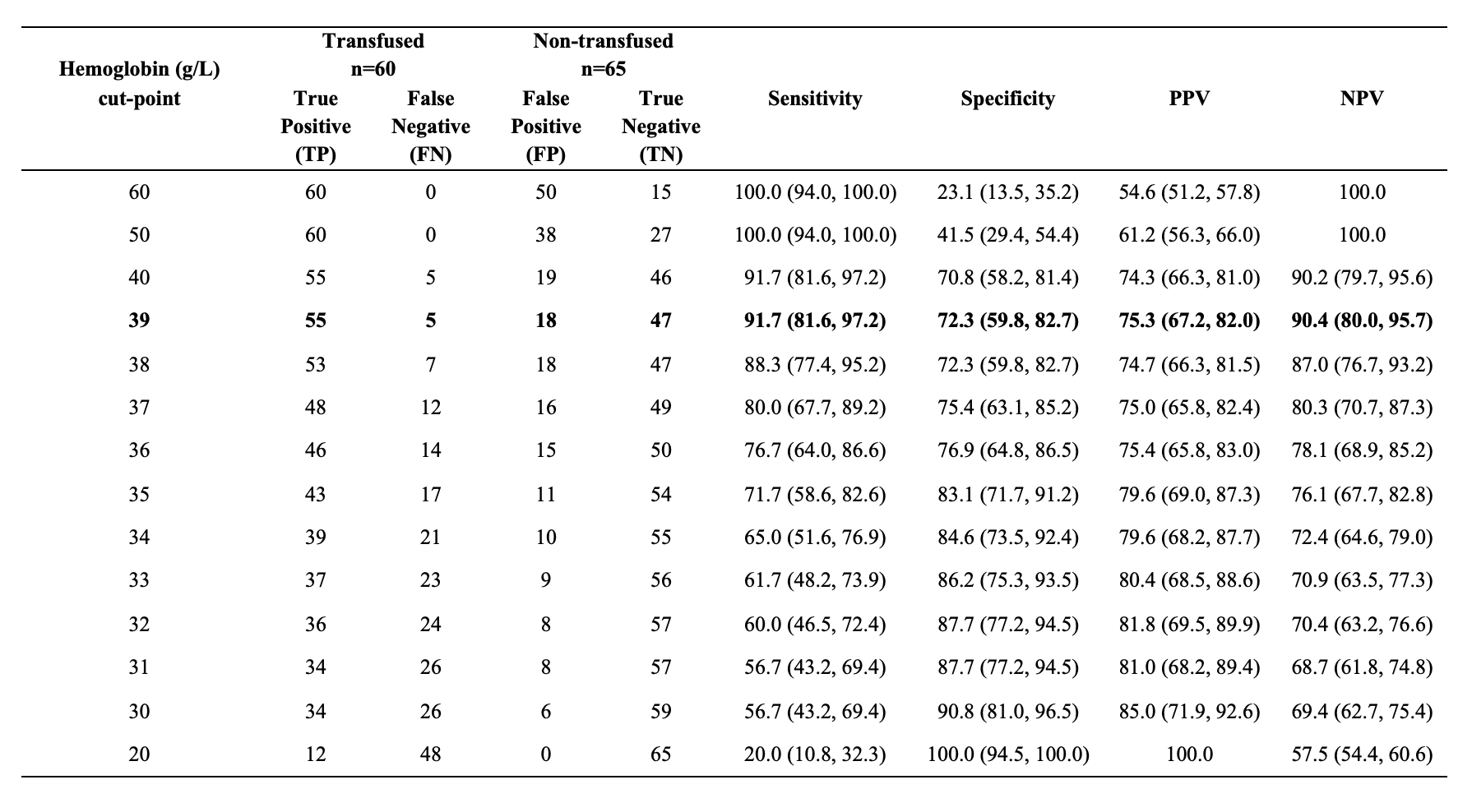
Design/Methods: This was an observational study of children 6-36 months, hospitalized with a primary diagnosis of IDA, abstracting data from hospital records. To examine predictors associated with transfusion versus non-transfusion, we created several models including initial hemoglobin level and measures of hemodynamic instability (initial heart rate, systolic blood pressure, Paediatric Early Warning System score). For each model, we conducted multivariable logistic regression to calculate odds ratios (OR), created receiver operating characteristic (ROC) curves and calculated the area under the curve (AUC) with 95% confidence intervals (CI).
Results: The sample included 125 children. Mean age was 18.5 (standard deviation 5.6) months and 79 (63%) were female. The AUC for the simplest model of hemoglobin level alone performed well in predicting transfusion (0.8862, 95% CI 0.8315, 0.9408). The AUC for measures of hemodynamic instability were < 0.70 (inadequate). The hemoglobin cut-point with maximal sensitivity (92%) and specificity (72%) was 39 g/L.
Conclusion(s): Hemoglobin level alone can predict receipt of an RBC transfusion in young children hospitalized with IDA. Measures of hemodynamic instability on their own did not adequately discriminate those that did or did not receive a transfusion, and when combined with hemoglobin, did not improve predictive power.
.png)
