Medical Education
Session: Medical Education 10
523 - Health Literacy Curricula in Pediatric Residency Programs: A National Survey
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 523
Publication Number: 523.3328
Publication Number: 523.3328
- NM
Nicole K. Meyers, MD (she/her/hers)
Pediatric Hospital Medicine Fellow
NewYork-Presbyterian Morgan Stanley Children's Hospital
New York, New York, United States
Presenting Author(s)
Background: Improving providers’ ability to communicate with populations having limited health literacy is a national priority in Healthy People 2030. Pediatric resident education on how to optimally communicate with children and families with limited health literacy is imperative, especially given the unique triad of patient, family, and doctor; however existing literature on resident health literacy education focuses largely on family and internal medicine training programs.
Objective: To describe the prevalence and characteristics of current health literacy education in pediatric residency programs nationally and barriers to implementation.
Design/Methods: Members of the Academic Pediatric Association’s Health Literacy Special Interest Group conducted a national, cross-sectional survey of associate program directors in 2022 via the Association of Pediatric Program Directors Research and Scholarship Learning Community. Our survey included questions on whether health literacy education is provided, educational strategies used, content highlighted, outcomes assessed, and barriers encountered. We used chi-square analyses for responder vs. non-responder demographics, descriptive statistics for quantitative results, and qualitative content analysis for written responses.
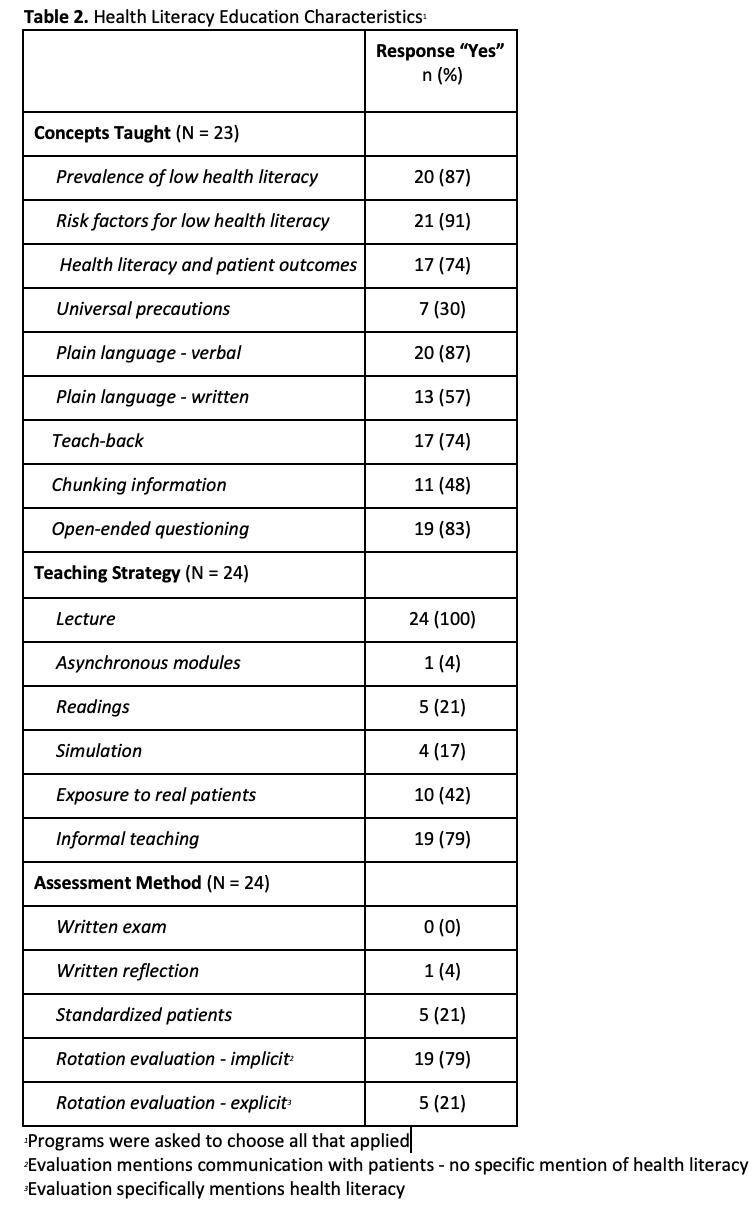
Results: Fifty-five APDs from 193 programs (29%) completed our survey. Responding programs varied in size, setting, and geographic region but significantly differed from non-responding institutions only in program size (Table 1). Of responding programs, 51 (93%) agreed health literacy concepts are important to include in residency education and 46 (84%) that residents would benefit from more health literacy training. Only 44% reported the presence of health literacy education and most without were uncertain about future plans to teach it. Barriers to implementation included time, competing priorities, and lack of local expertise and resources. Among programs with health literacy education, there was great variability in concepts taught, teaching modalities, and evaluation methods (Table 2).
Conclusion(s): Almost half of responding programs do not currently teach health literacy and of those that do, there is considerable variability, representing a gap in pediatric resident education. Future directions include development of a standardized, accessible health literacy curriculum that can be adapted to specific pediatric programs’ needs.
.png)